An Immunologist Fights Covid with Tweets and a Nasal Spray

Akiko Iwasaki, an immunology researcher at the Yale School of Medicine, contributes to the fight against Covid-19 with both her vaccine work and her explanations of pandemic science for the public on social media.
Brandon Schulman for Quanta Magazine
Introduction
In the United States and some other countries, the Covid-19 pandemic has entered a paradoxical stage in which the coronavirus has evolved into a highly contagious variant and sent cases soaring, but the public’s attitude has evolved toward indifference, deflating precautionary measures.
Immunologists like Akiko Iwasaki of the Yale School of Medicine, keenly aware that the consequences of the unfinished pandemic are still playing out, continue to combat the virus in the lab. “The enemy has evolved, and the world needs next-generation vaccines to respond,” Iwasaki recently wrote in an op-ed column for The New York Times. Although current vaccines against the coronavirus are highly effective at preventing severe disease and death, they are less successful at preventing infection. Vaccines in the form of a spritz up the nose could change that, Iwasaki said, by heading off infections and the array of symptoms known as “long Covid” that linger for many former patients.
Iwasaki’s group at Yale, like other laboratories around the world, is developing such nasal sprays. She and her team are also trying to tease apart the mystery of long Covid and why only some people are afflicted with it.
The pandemic “has transformed my own science,” said Iwasaki, who like many other researchers reoriented her lab toward studies of the coronavirus at the start of the pandemic. Previously, much of her laboratory’s work had looked at how the portion of the body’s defenses called the innate immune system detects viruses and how that helps to prime the immune responses in mucous membranes.
Around that same time, in March 2020, Iwasaki found the boundary between her job and her personal life dissolving, because what had been niche conversational topics about immunology with colleagues and students suddenly became of great interest to the public. With a deluge of alarming reports about Covid flooding the news, Iwasaki found herself becoming a lifeline for the worried and the curious who came to her on Twitter with questions.
She teaches on social media, and knocks down misinformation, with the same fervor that she brings to her research — and is eminently qualified for both battles. In 2018, Iwasaki was elected to the National Academy of Sciences and in the following year to the National Academy of Medicine. In 2021, she was elected to the European Molecular Biology Organization and to the American Academy of Arts and Sciences. She is also leading a newly launched Yale Center for Infection and Immunity that will expand her research into diagnoses, treatments and nasal vaccine development for infectious diseases.
Quanta spoke with Iwasaki about the evolution of the pandemic, her efforts to teach the public and why she thinks the nasal spray may be the new weapon that we need. The interview has been condensed and edited for clarity.

Iwasaki examines slices of brain tissue on exhibit at the Cushing Center at Yale University.
Brandon Schulman for Quanta Magazine
Could nasal sprays change how we fight this pandemic and the future ones?
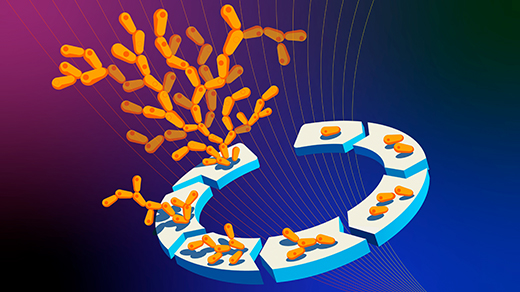
I think it’s going to fundamentally change the way we approach vaccines against pathogens, especially the ones that are coming through mucosal surfaces like the nose. We can apply the same strategy to other respiratory pathogens, like the influenza virus, adenovirus or the rhinovirus. What we need to do is to take advantage of the regular, intramuscular vaccine as a primary vaccine and piggyback onto that with a nasal spray.
How would that work?
After someone is vaccinated with one of the available intramuscular vaccines, you just spray a simple protein, a recombinant spike protein, into the nose. And that converts the systemic immunity [from the injection] into mucosal immunity. The strategy is called “prime and spike.”
The key is that we are taking advantage of the existing immune response by the T cells that people have from previous vaccinations. That means we don’t have to use any adjuvant, or extra molecule, to stimulate an immune response, which is advantageous because it minimizes unwanted side effects.
Why are mucosal surfaces good places to elicit immune reactions?
Mucosal surfaces are the wet surfaces that line your nasal cavity, oral cavity, your genital tract or gastrointestinal cavity. It’s where most pathogens enter our bodies unless you get exposed to them through a cut or a vector like a mosquito or a tick. It’s the first line of defense against pathogens.
If mucosal surfaces are a first line of defense to pathogens, why don’t current Covid-19 vaccines target them?
Well, that’s a great question; we wonder the same thing. Most vaccines are given into a muscle with a needle. And those vaccines are really good at inducing systemic and circulating immune responses. But they’re not designed to elicit mucosal immunity. That is not part of the vaccine design right now. We’re trying to change that.
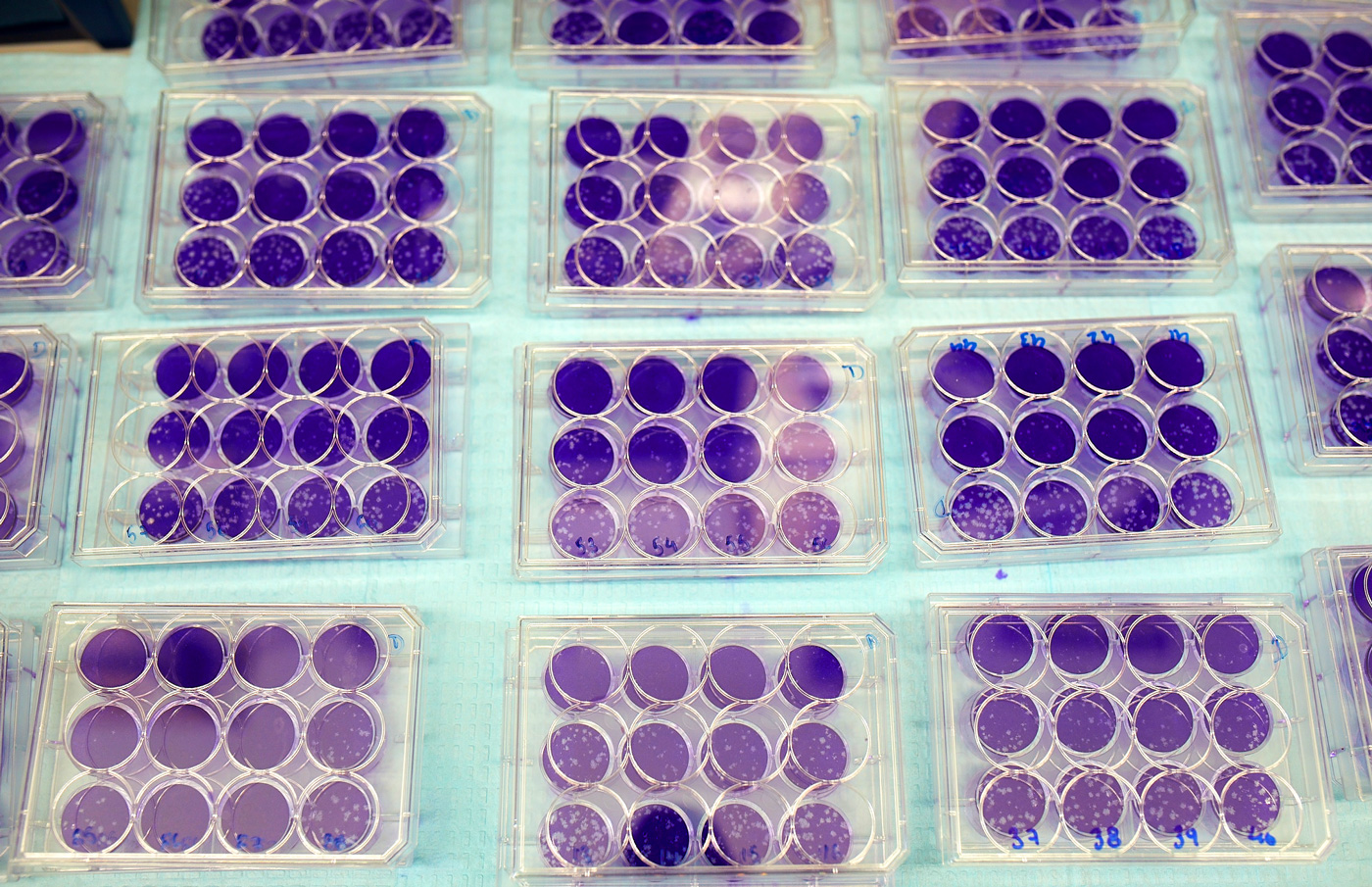
Viral plaque assays, in which fluids contaminated with viruses are spread on cells growing in culture, enable Iwasaki and other immunologists to quantify how much virus is present in a sample.
Brandon Schulman for Quanta Magazine
When I was growing up, I remember there being an option to get a flu vaccine as a nasal spray. Is this the same idea?
Exactly. So that is called FluMist and it’s given to people between 2 and 49 years of age. It works really nicely because it induces this local immune response. But as with all other flu vaccines, it’s always a gamble trying to guess the right antigen. With the coronavirus, you don’t need to guess anything — you know exactly what you need.
And that is to target the coronavirus spike protein?
Yes. The spike protein is the target, but it will change as variants arise. Instead of chasing the next variant, we want to generate a broadly reactive immune response to current variants that can also cross-react with future variants. This can be achieved by using a different spike protein. We used SARS-CoV-1 spike protein for this purpose.
Would nasal spray vaccines be as effective as the intramuscular vaccines currently being used to battle the virus?
I would think that it will be more effective. We still have to test it in humans, but because the spray vaccine establishes local immunity where the virus enters the body, people may not get infected from the pathogen, which is very different from the intramuscular vaccines where we’re preventing severe disease. If you don’t get infected, of course, you avoid any downstream consequences, like long Covid.
Another advantage is that it’s a nasal spray, so you don’t necessarily rely on health care personnel to deliver it. You may just get it from your local pharmacy and administer it yourself. That also expands the scope to other countries that may not have the workforce to deliver intramuscular vaccine but may have the capacity to deliver nasal spray. It’s also very easy to produce: It’s just a recombinant protein that can be stored in the fridge for a few months.
I hate needles!
Many people do. And they may find a nasal spray much more amenable.
Would the nasal spray also somehow build up immunity in the mouth, which is another place through which we can be infected?
That is something we are looking at right now in hamsters. We hope to find the answer soon.

“When the pandemic hit, it was kind of natural for me to start teaching those who are interested,” Iwasaki said.
Brandon Schulman for Quanta Magazine
What are the challenges of getting mucosal vaccines to work? Why don’t we have one already?
The challenge of getting mucosal vaccines is that the mucus layer blocks the uptake of antigens and vaccines, making it a difficult barrier to deliver vaccines. That is why most existing mucosal vaccines are based on weakened forms of live viruses that have their own strategy to penetrate the mucus layer and produce antigens. Our “prime and spike” approach does not require replicating or live pathogens. Even a small amount of the recombinant spike is enough to trigger robust immunity because we are leveraging memory T cells from the previous vaccine to activate antigen-presenting cells in the mucus layer.
Are there candidate mucosal vaccines for the coronavirus that are already in clinical trials? When would you predict that such vaccines will be released?
Yes, several are in clinical trials. Depending on the results, I am hoping that some of these can be approved for human use soon.
Your lab is also focused on understanding what causes long Covid, right?
We are putting our effort now into trying to understand long Covid, yes. Long Covid is a debilitating condition for millions of people now. It’s estimated that 10% to 30% of people get long Covid after infections.
It has over 200 associated symptoms, involving every organ system. Some people have a couple of them, while others have over a dozen. Some people recover after several weeks, and others do not. So it’s a very heterogeneous disease, but there are four hypotheses we are testing now to see what people are actually suffering from.
What are the four hypotheses?
It could be viral remnants or an infectious pool of viruses hidden somewhere in the body that’s still causing symptoms but not leading the person to test positive on PCR tests. It could be autoimmunity or immune system cells themselves that are driving the symptoms. It could be the reactivation of other silent viruses or microbiome changes. Or tissue damage from the infection or treatment may be lingering or turning into fibrosis or chronic disease.

“Immunology as a discipline is a very deep field; we will never understand everything,” Iwasaki said. “I think that this pandemic has highlighted a few things that we still need to work on.”
Brandon Schulman for Quanta Magazine
People with chronic fatigue syndrome have similar symptoms, right?
Exactly. People who have been suffering from chronic fatigue syndrome over the years have been largely ignored or dismissed. Many doctors kind of think that this is a psychiatric disease instead of something that’s happening outside the brain. I think that this whole viewpoint needs to change. And there are so many other pathogens that lead to these kinds of post-infectious syndromes. So I don’t want people to think of this as a unique feature of Covid.
You quickly became a leading and guiding voice during the pandemic. Did that happen organically?
I’ve always loved teaching. I’ve been teaching immunology at Yale for a long time now. And, you know, teaching is also learning. I do a lot of reading to catch up with all the different advances in immunology, and oftentimes I pick up things that I didn’t know before. Students’ questions also trigger me to investigate what we don’t yet understand in immunology. So, when the pandemic hit, it was kind of natural for me to start teaching those who are interested.
Before the pandemic, I had a Twitter account where I was tweeting about immunology or issues with academia and women in science, things like that. I would post Twitter threads about our lab’s work and a few immunologists would like the post. But there was a huge switch in the general public’s interest in viruses and immunity once the pandemic hit. People outside of immunology became very interested in our work — not only other scientists but also the general public, journalists and reporters. All of a sudden, people wanted to learn about the immune system and how it works, and people started talking about antibody levels and T cells. This transition happened pretty much over March 2020. I think the first thing that really kind of put me on the stage was this Tweetorial [a tutorial as a Twitter thread] that I did about a video I made called “Immunology 101 for non-immunologists,” just to describe what the immune system does.
“There’s a lot of stereotypes against women in science and implicit biases that are working against us,” said Iwasaki, who has become a prominent advocate and mentor for women and minorities in science.
Brandon Schulman for Quanta Magazine
You also do a lot to advocate for women and minorities in science. Where did your passion for that come from?
I grew up watching my mother suffer from this kind of injustice. She worked at a radio station. At that time, when women became pregnant, to some extent they were expected to quit their job. She has three daughters, and every time she would have the babies, people pressured her to leave the company. She’s been jeered at and harassed and faced horrible things. But she never quit the company and instead formed a sort of network of other women and men to fight for the right to work. Watching this and hearing about it really influenced me to think that we need to stand up. There’s a lot of stereotypes against women in science and implicit biases that are working against us.
Is your mom your role model?
Absolutely, yes, she is. And so is my father.
You’re a role model for the younger generation as well. I saw on your Twitter account a photo of a fourth grader presenting about long Covid with inspirational quotes from you.
That was such a heartwarming post. I loved it. I’m just so delighted that people looking at me are thinking about science and thinking about immunology. It’s amazing that a young person like that is thinking about long Covid and research. And that is just so inspirational for me in return.
Did you always know you were going to be an immunologist?
I didn’t know that. I grew up in a very progressive household, where my parents encouraged me to pursue whatever I wanted. It was in high school that I met a math teacher who instilled this interest and excitement for math in me. I started taking more math classes and decided that maybe I’ll go into science instead of literature, which is what I wanted to do before that. I left Japan when I was 16 to explore the world and see what’s out there. I finished high school in Canada, and then I went to undergraduate and graduate work at the University of Toronto, which was really formative for me in trying myself out in a different environment. That’s also where I learned the joy of immunology, starting in my senior year when I took an introductory course and learned about how vaccines work and how they save millions of lives. I thought, wow, what could be more interesting and fulfilling than to study the immune system?

Brandon Schulman for Quanta Magazine
If you went back to that class today, do you think that the teachings would be very different?
Oh yeah, I hope so. We’ve learned so much since then. When I took that class, the innate immune system wasn’t really understood well. It was only in 1997 that Ruslan Medzhitov, who is now my husband, in Charlie Janeway’s lab figured out that innate signaling through recognition of pathogen-associated molecular patterns is what triggers adaptive immunity. That revolutionized the way we think about how the pathogen is being recognized by the immune system. That’s the basis of adjuvants. Back then, we had no idea about these things. It was not taught at all.
Even now, though, how much do we understand the immune system? Are there still major gaps that need to be filled?
Immunology as a discipline is a very deep field; we will never understand everything. So I think that this pandemic has highlighted a few things that we still need to work on, one of which is mucosal immunity. It’s been a subfield of immunology that hasn’t gotten a lot of public attention. And then what are the molecular pathways and trafficking patterns? All these things are worked out for some tissues, like the gut, but not in the respiratory tract.
We’re now in this weird stage of the pandemic, where it feels like it’s over but it’s really not. Where do we go from here?
You know, one of the things that worries me is the evolution of the virus and the variants that are continuously emerging. If the future variants are very immune-evasive or pathogenic, we would have to think about how we are living these days. Many people have decided that Covid is over, and they’re just unmasking and not bothering to get vaccinated. That’s unfortunate, because I think those are the people that are going to be most vulnerable to a future wave of infection.
Are we ready for the next pandemic?
We’re still failing to respond appropriately to the current pandemic. People have this sort of pandemic fatigue. They’re just done with it, regardless of the risk that they’re facing. So if something were to hit right now, I’d be worried because people are intolerant to taking any more measures. And that is a perfect storm for the virus to spread and make people sick. So yes, I just hope we have some break.
Are you or others in the field worried about the spread of monkeypox? Could it ever become a massive worldwide problem like smallpox was?
I am not certain how effectively monkeypox can spread to become a massive pandemic like smallpox. If we can implement testing, isolation, contact tracing and vaccination measures quickly before that happens, a massive pandemic can be prevented.
Would nasal sprays work for monkeypox?
For monkeypox, the nasal cavity is not a major site of mucosal transmission. It may also be transmitted via broken skin, sexual contact or other routes. We’re still finding out how many ways this virus transmits. So I would not think a prime-and-spike type of vaccine is best for this virus.