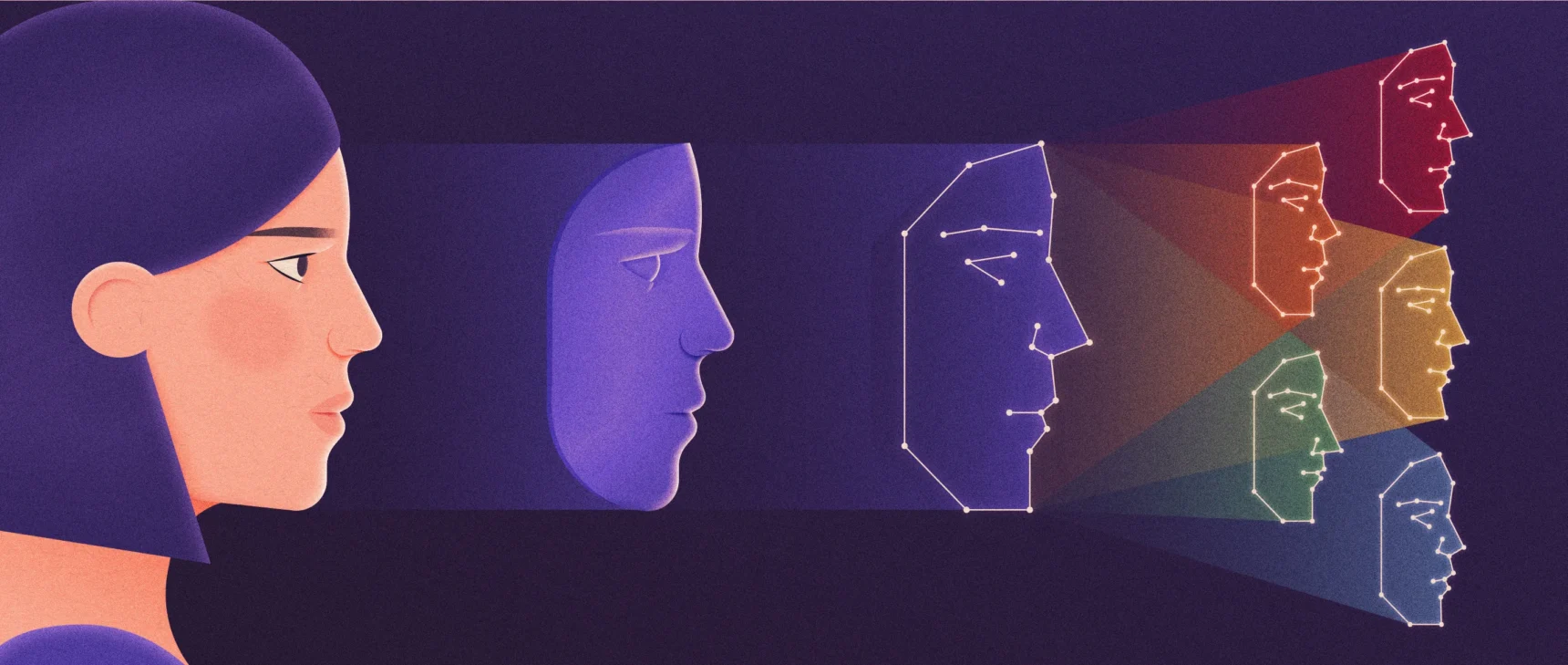
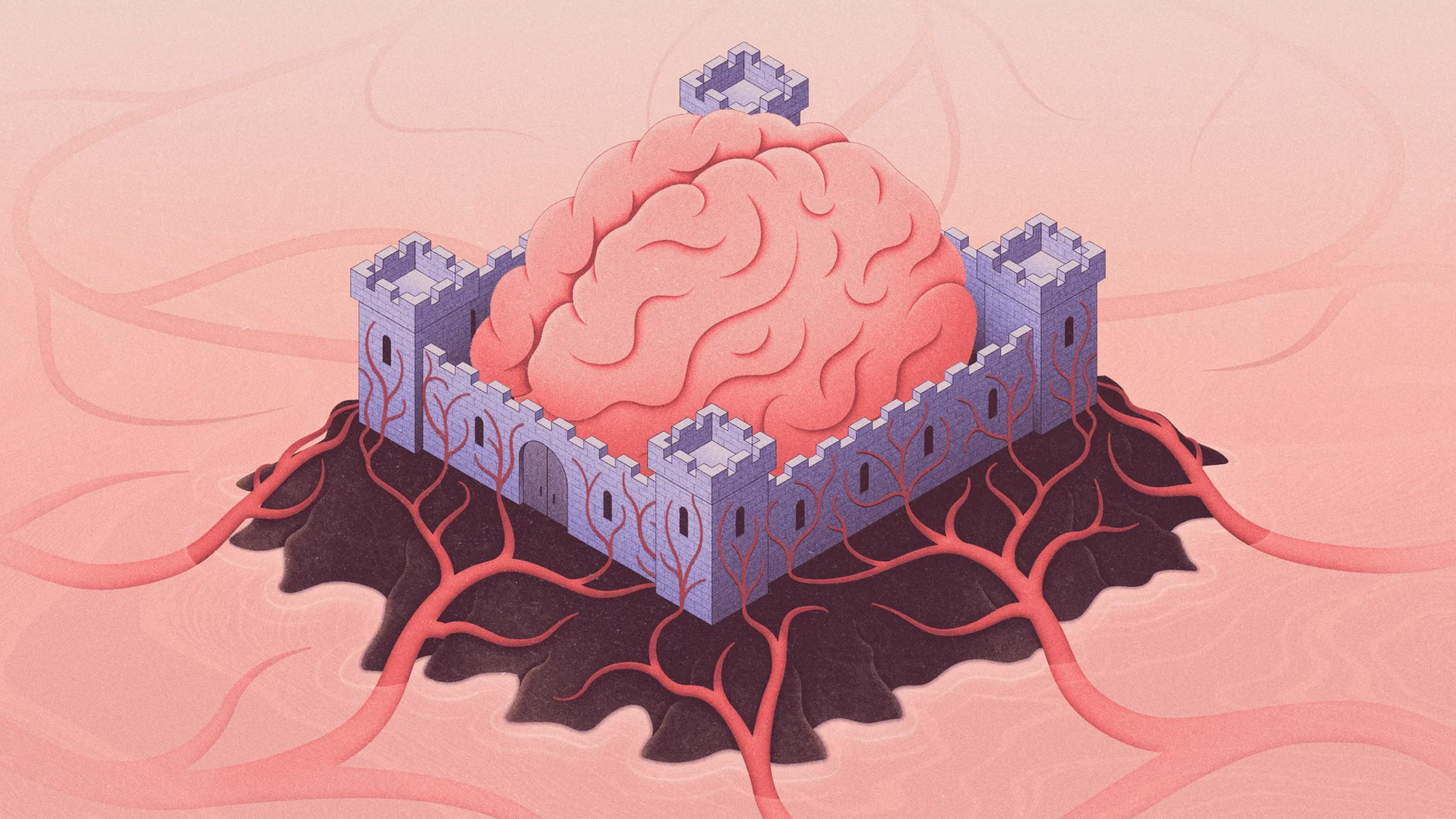
How the Brain Protects Itself From Blood-Borne Threats
Kristina Armitage/Quanta Magazine
Introduction
Enough pints of beer can have you falling off your bar stool or loudly reciting lyrics to early 2000s jams to total strangers, because alcohol can get past one of the strongest defenses in the body. If you’ve ever been drunk, high or drowsy from allergy medication, you’ve experienced what happens when some molecules defeat the defense system called the blood-brain barrier and make it into the brain.
Embedded in the walls of the hundreds of miles of capillaries that wind through the brain, the barrier keeps most molecules in the blood from ever reaching sensitive neurons. Much as the skull protects the brain from external physical threats, the blood-brain barrier protects it from chemical and pathogenic ones.
While it’s a fantastic feat of evolution, the barrier is very much a nuisance for drug developers, who have spent decades trying to selectively overcome it to deliver therapeutics to the brain. Biomedical researchers want to understand the barrier better because its failures seem to be the key to some diseases and because manipulating the barrier could help improve the treatment of certain conditions.
“We’ve learned a lot over the last decade,” said Elizabeth Rhea, a research biologist at the University of Washington Medicine Memory and Brain Wellness Center. But “we’re definitely still facing challenges in getting substrates and therapeutics across.”
Protection, but Not a Fortress
Like the rest of the body, the brain needs circulating blood to deliver essential nutrients and oxygen and to carry away waste. But blood chemistry constantly fluctuates, and brain tissue is extremely sensitive to its chemical environment. Neurons rely on precise releases of ions to communicate — if ions could flow freely out of the blood, that precision would be lost. Other types of biologically active molecules can also twang the delicate neurons, interfering with thoughts, memories and behaviors.
“It’s really there to control the environment for proper brain function,” said Richard Daneman, an associate professor of pharmacology at the University of California, San Diego.
So the blood-brain barrier provides protection, but it’s not a discrete structure like the walls around a fortress. Instead, the term refers to the unique properties of the blood vessels in the brain and those of the neighboring brain cells that wrap closely around those vessels.
Most of the body’s capillaries are “leaky” at a molecular level to allow the free flow of nutrients and other substances. Their permeability is crucial to the function of organs such as the kidney and liver.
But the brain’s blood vessels are built to a higher, less leaky standard. The endothelial cells that make up the capillary walls are pinned tightly together by structures called tight junctions. Thin parallel protein strands stick the cells together like “wires through the bricks,” said Elisa Konofagou, a professor of biomedical engineering and radiology at Columbia University. A few kinds of molecules can get past, but in small amounts. And they are mostly very small and water-soluble.
But the brain also needs many other molecules such as glucose and insulin, which can’t squeeze between the tight junctions. The barrier is therefore also lined with pumps and receptors that, like bouncers for an elite club, permit only certain molecules in — and quickly eject most trespassers. Beyond the capillary wall itself are layers of supportive cells including pericytes and astrocytes, which also help to maintain the barrier and adjust its permeability.
Nevertheless, despite all those layers of protection, some unwanted substances do get through to the brain reliably. Ethanol, the main ingredient in alcoholic beverages, can simply diffuse through cell membranes. Some molecules look too much like the needed ones to be kept out. If you’ve ever wondered why over-the-counter antihistamines for allergies make you sleepy, it’s because they slip through the barrier and get to your neurons. (Newer, non-drowsy antihistamines don’t penetrate the barrier and act only on immune cells in the blood.)
The blood-brain barrier is “there to deliver what the brain needs,” Daneman said. But not every part of the brain needs the same molecules, so the barrier is not the same everywhere. The barrier in the olfactory bulb, for example, acts differently and has a different protein composition than the barrier in the hippocampus, Rhea said.
Merrill Sherman/Quanta Magazine
In fact, some parts of the brain don’t have a traditional blood-brain barrier at all. In the choroid plexus, a tissue in the large cavities of the brain that produces cerebrospinal fluid (CSF), the walls of blood vessels are much leakier. They have to be because the “blood-CSF” barrier of the choroid plexus needs to secrete half a liter of CSF into the brain every day, and that kind of output requires extensive amounts of water, ions and nutrients from the blood.
Even though this protective function isn’t perfect, it is so universally useful that every organism with a complex nervous system has something resembling a blood-brain barrier, Daneman said.
Even flies and other insects, which don’t have blood vessels, have one. Their equivalent of blood simply sloshes through organs inside their exoskeleton, but their equivalent of a brain is sheathed in protective glial cells.
An ‘Ozone Layer’
When the barrier breaks down, it brings a wave of trouble to the brain. The blood-brain barrier “is like the ozone layer for the Earth,” said Berislav Zlokovic, chair of the department of physiology and neuroscience at the Keck School of Medicine of the University of Southern California. Just as opening a hole in that thin atmospheric layer caused harmful radiation to flood the planet, opening up the blood-brain barrier can cause harmful molecules to flood the brain.
Many groups are examining how the barrier changes during disease or injury. A breakdown of the blood-brain barrier is a hallmark of Alzheimer’s disease, for example. A recent study in the journal Nature Neuroscience mapped out significant changes to gene expression within blood-brain barrier cells in the brains of Alzheimer’s patients. In multiple sclerosis, the blood-brain barrier breaks down, leading to an overflow of immune system cells in the brain that then attack the protective insulation around neurons. Traumatic brain injuries and strokes can also open up the barrier and cause potentially irreversible damage.
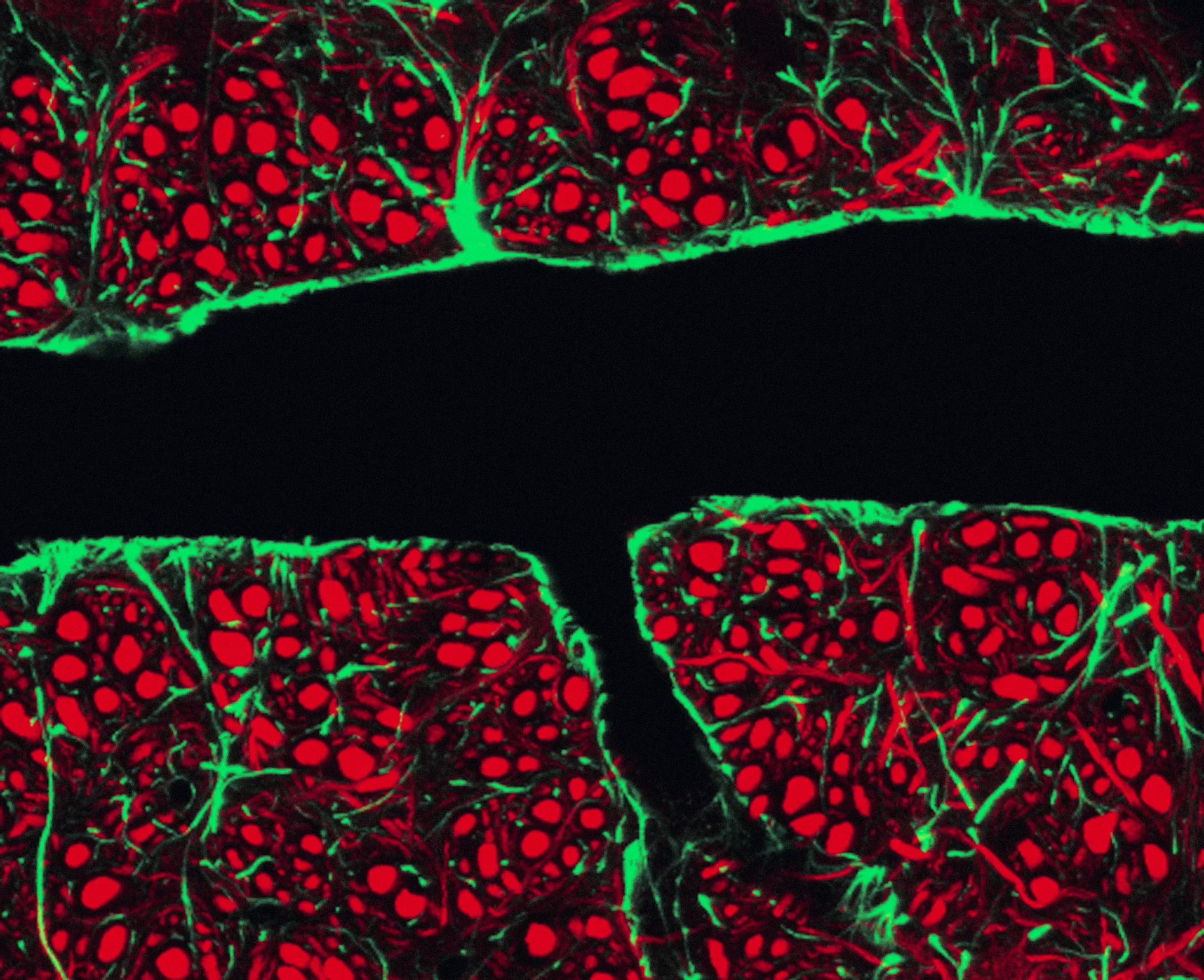
The tightly packed cells that line blood vessels in the brain make the blood-brain barrier possible. In this micrograph, the black indicates the interior of the vessel where the blood would flow.
C.J. Guerin, PhD, MRC Toxicology Unit/Science Source
Selectively opening or closing the blood-brain barrier could be beneficial, however. Many potentially useful drugs can’t get past the barrier. That’s partly because a lot of the progress in studying the blood-brain barrier was hindered by technical limitations, many of which have since been overcome with new technologies, said Maria Lehtinen, chair in pediatric pathology research at Boston Children’s Hospital. “I think this is a really exciting time for the field.”
In recent years, many groups have zeroed in on a “Trojan horse” approach in which drugs piggyback into the brain by holding onto molecules that can naturally transit the barrier. Other work has looked at using targeted ultrasound to open up parts of the barrier and deliver drugs to treat Parkinson’s disease and other ailments. In a recent study in Science Advances, for example, researchers successfully delivered fluorescent proteins into the brains of macaques by opening the blood-brain barrier with ultrasound. They are now working to adapt that approach to the delivery of gene therapy drugs that could fight Parkinson’s disease.
Where once the blood-brain barrier was thought of as a static, unchanging wall, scientists now view it as dynamic and “living,” Lehtinen said. It likely “grows and develops in different ways in different parts of the nervous system.” It temporarily creaks open naturally when we are in deep REM sleep or when we exercise. It changes with exposure to hormones and drugs, closing off old avenues for entry or opening new ones. When some molecules bind to the barrier, its cells can sometimes signal to the brain how to act without ever letting the molecule through, Rhea said.
So rather than a stone rampart around a medieval fortress, the blood-brain barrier is like a magical wall in which doors appear and disappear, and windows grow bigger and smaller. Some parts crumble, some parts get built back — and it is constantly changing.
The blood-brain barrier is “never static,” Rhea said. “It’s never just this wall that needs to be overcome.”
Editor’s note: Maria Lehtinen is an investigator with the Simons Foundation’s Autism Research Initiative (SFARI) and Richard Daneman has previously received funding from the Simons Foundation. The Simons Foundation also funds Quanta as an editorially independent magazine. Funding decisions have no influence on our coverage.