The Contrarian Who Cures Cancers
James P. Allison shared in a 2018 Nobel Prize for his discoveries about the immune system and his development of therapies that free up the immune system to attack cancers more aggressively.
Elizabeth Conley for Quanta Magazine
Introduction
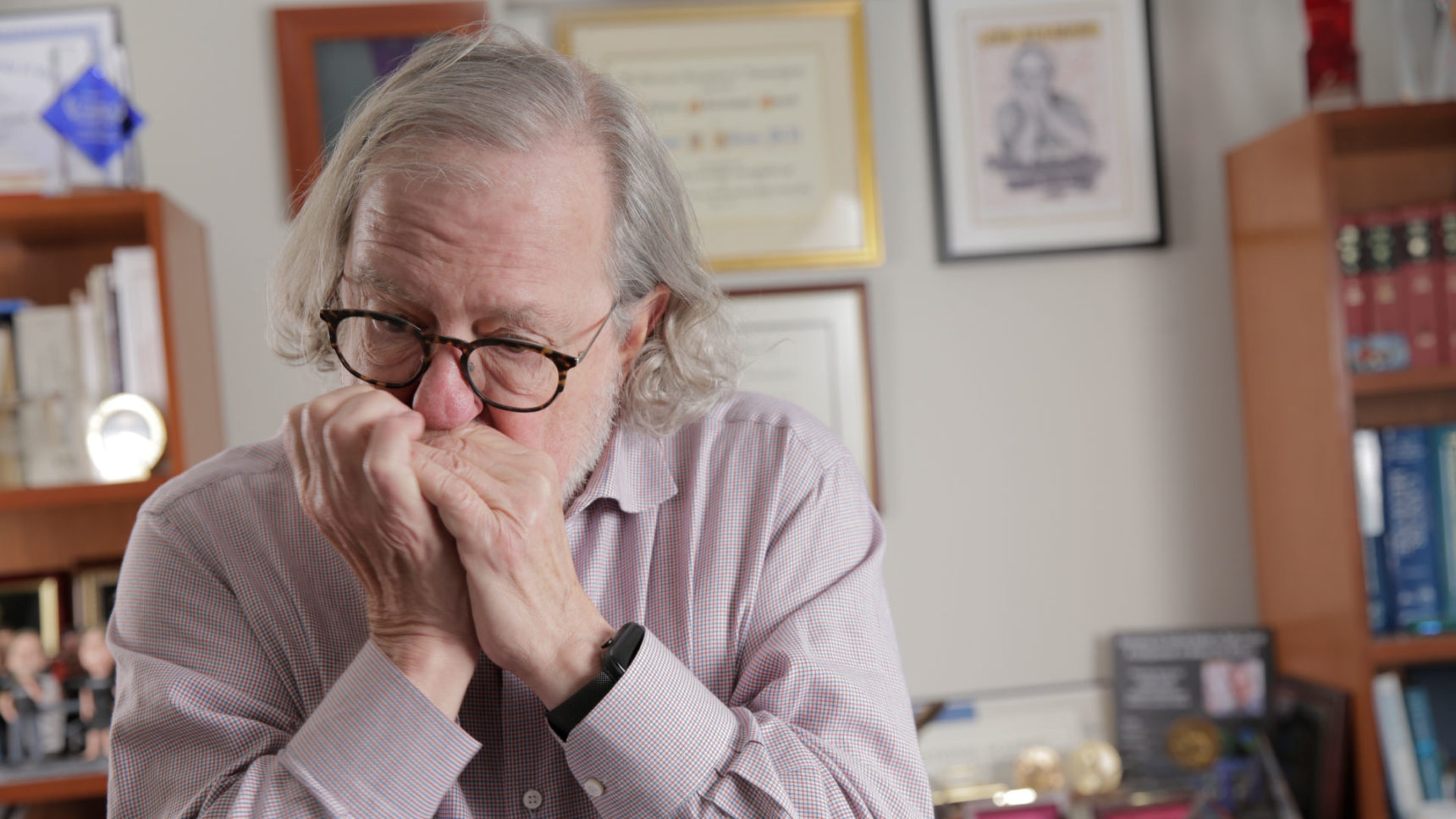
When I first met the immunology researcher James P. Allison in 2014, he was just becoming an icon. Columbia University had brought him to its campus to present him with the Louisa Gross Horwitz Prize for the new type of cancer therapy he had developed. Instead of trying to burn, poison or surgically remove malignant cells from the body, his treatment mobilized a patient’s immune system to destroy them.
During his talk at the award ceremony, Allison explained that three years earlier, the Food and Drug Administration had approved the antibody drug he had developed, ipilimumab, for use against late-stage metastatic melanoma, which is among the deadliest of cancers. Some of the terminal patients who had participated in earlier trials, he reported, had gained a decade of life. As he described how his drug had changed the prognosis for some of these patients — it was effective for about 20% of them — tears came to his eyes.
In all my years on a science beat, I’d never seen a researcher cry. Allison, with his long gray hair and his loose-fitting clothes, struck me as among the most interesting figures in the scientific world. Speaking with him later, I sensed that he was someone deeply original, extremely confident of his intellectual powers and unafraid to go where they took him — the exact qualities it takes to invent a paradigm-shifting cancer treatment.
Allison’s drug wasn’t the first or only form of immunotherapy; scientists have worked on anticancer vaccines, for example, for decades. What made Allison’s “immune checkpoint therapy” unique was that it used antibodies to unlock the immune system’s potential to kill cancer cells.
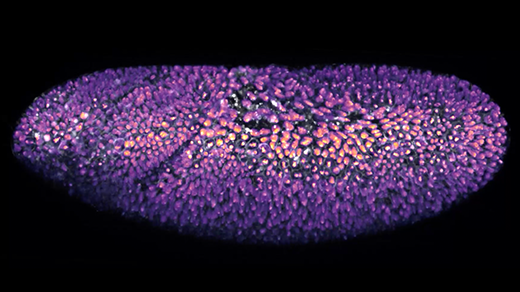
This approach is the culmination of Allison’s highly accomplished immunology career. In the early 1980s, he identified the receptor that allows the immune system’s T cells to recognize the antigens of infected or abnormal cells. A decade later, he showed that T cells also need a signal from a “costimulatory” molecule to launch their attacks. Then Allison and his colleagues discovered that a molecule called cytotoxic T lymphocyte antigen-4 (CTLA-4) acts as a checkpoint, or built-in brake, on T cells. They could remove the brake and set T cells loose against cancer cells with an antibody — ipilimumab — that inhibited the CTLA-4 checkpoint.
Work on immunotherapy has become a major trend in biotech research in the past decade. Variants and extensions of immune checkpoint therapy, often in combination with other drugs, are the basis for many treatments under development for cancers of the brain, lung, bladder and kidneys. None of these immunotherapy drugs are yet effective for all patients or all cancers, but when patients respond — as many metastatic melanoma patients do — their longevity is significantly improved.
Allison, now 71, was emphatic in his assessment of those outcomes when I spoke with him in his office at the University of Texas MD Anderson Cancer Center, where he is the chairman of the department of immunology and the executive director of its Immunotherapy Platform. “You don’t just get an increase in median survival,” he said. Thousands of patients treated with immunotherapy have lived cancer-free for 10 or more years. “These people have been cured.”
Such results have brought Allison not a few honors, including the Paul Ehrlich and Ludwig Darmstaedter Prize and the Lasker-DeBakey Clinical Medical Research Award in 2015 and the Wolf Prize in Medicine and the Balzan Prize in 2017. Then, in 2018, Allison shared the big one with Tasuku Honjo of Kyoto University: the Nobel Prize in Physiology or Medicine (Honjo had independently found a different cancer checkpoint).
At MD Anderson, Allison’s colleagues were so thrilled that they held a victory parade for him. In Houston, Allison has become a major celebrity: a sought-after guest at fundraising galas, an advocate with the Texas legislature for research dollars, and the target of countless autograph hounds and selfie seekers. It hasn’t hurt his celebrity standing that on occasion he also plays harmonica on stage with Willie Nelson and that a documentary about him and his work, Jim Allison: Breakthrough, was released last year.
Allison and I spoke in person and over the phone, and also corresponded by email in the course of this reporting. The interview has been condensed and edited for clarity.
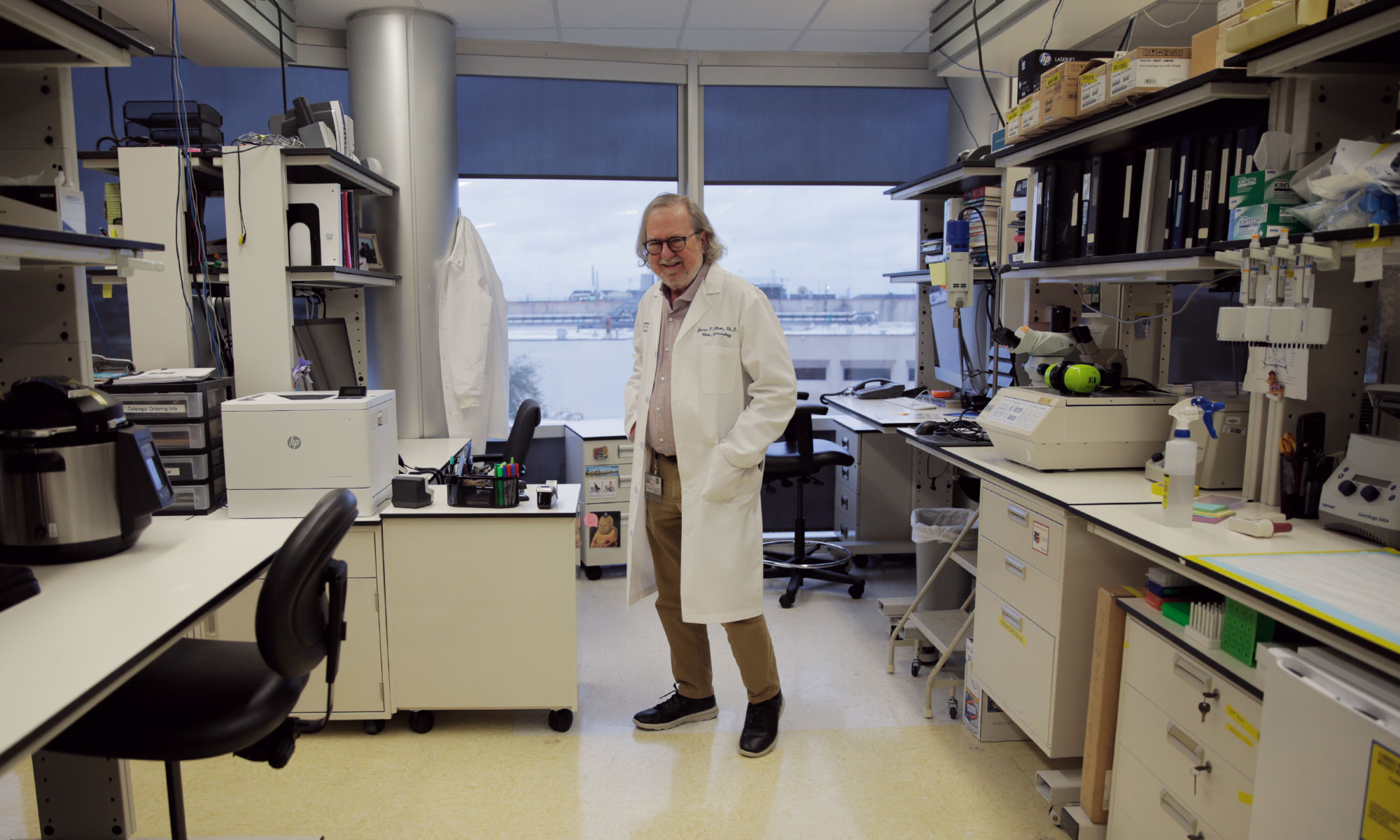
Jim Allison in his laboratory at the University of Texas MD Anderson Cancer Center in Houston.
Elizabeth Conley for Quanta Magazine
We met five years ago, before all the acclaim and honors. At the time, you seemed overworked and exhausted. Today, you are looking slimmer, tanner, rested. Does winning a Nobel Prize improve one’s health?
[Laughs.] Yeah. Five years ago, I was eating too much, drinking too much, traveling too much. I decided that it was time to quit doing that. I started eating better, drinking less and saying no to some demands. I’ve never been good at saying no.
You know where all that started? A year ago, in Stockholm, when we went for the Nobel Prize. The celebrating started every morning at 11 with champagne. It would go until midnight — except on the night of the ceremony, when it went till 6 a.m. I gave out at 5.
That’s when I decided it was time to take better care of myself.
Aside from pushing you to embark on a wellness campaign, how has winning the Nobel Prize changed your life?
Well, I get a lot more invitations to do things than I used to. I try to accept the ones where there’ll be an audience that would be useful to talk to. I want them to know immunotherapy is working.
On the other hand, I’m learning how to say no to nonessential invitations more often. A lot of the Nobel laureates tell me this can become a problem. But the truth is, I like talking about immunotherapy. I like spreading the word. I’ll say yes to school groups or if I’m needed to talk to Congress about more money for cancer research.
Has the Nobel made you a bit of a celebrity?
Oh, yeah. For a while, right after the ceremony, I couldn’t get into my office because in the morning people would be waiting for me so that they could take selfies and get autographs and stuff.
But I’ve got to say this: For better or worse, the Nobel and the other prizes have validated immunotherapy — specifically, the checkpoint-blockades way of treating cancer. The Nobel and the other awards have validated the notion that cancer can be cured. That wasn’t the paradigm before. For the longest time, what we were doing was sort of at the edge of credibility.
What do you mean?
Well, even after “ippy” — ipilimumab, the first immunotherapy drug, which I developed — was approved by the FDA for melanoma, there were colleagues naysaying it. There’s one person — I won’t say his name here — who all along insisted it would never work. Then in 2011, after ippy was approved by the FDA for melanoma, he went, “Well, it’ll be a good melanoma drug, but it won’t work in anything else.”
For whatever reason, there’s sometimes been a lingering skepticism. But the situation for immunotherapy is much different from 15 years ago. In those days, 90% of people I encountered thought it was not worth doing because it wouldn’t work.

Allison confers with members of his laboratory team.
Elizabeth Conley for Quanta Magazine
I’d go, “I’ve got something that can cure cancer,” and they’d go, “What kind of cancer would you use it for?” I’d say, “I don’t think the [specific] cancer matters much,” and that would be the end of the meeting. There had been a lot of failures with attempts to make vaccines for cancer. No one wanted to go there.
I went to the various pharmaceutical companies for two years, and only one small company, Medarex, was eventually interested. Medarex was later [in 2009] bought by Bristol-Myers Squibb, which took ippy through the approval process and to market.
Immunotherapy is said to be the first major change in cancer treatment in 100 years. Do you think some of the skepticism had to do with how different it is from what had become the standard treatment — usually some combination of surgery, radiation and chemotherapy?
That may be part of it. These drugs target the immune system, not the cancer. They unleash the immune system so that it will destroy the cancer. The drugs are based on the idea that our adaptive immune system can recognize and destroy our own abnormal cells.
And the treatment works! More than 20% of the metastatic melanoma patients who get it achieve a long-lasting response. It used to be that with metastatic melanoma, the average time between diagnosis and death was something like four months. We’re seeing some melanoma patients living 10, 20 years after being diagnosed. There’s a woman who was in on the very beginning of the phase 1 trials with ippy. She’s 19 years out now.
After the trials were expanded, thousands of others received it, and a lot of them have lived 10-15 years so far, with no reoccurrence.
Is 20% good enough?
No. It’s not an endpoint. The research is continuing. We’re still in the early days of immunotherapy.
With metastatic melanoma, right now, with ipilimumab alone, the response is, as I mentioned, 20-something percent. With a drug that acts on PD-1 [programmed cell death protein 1], a different immune checkpoint found independently by Tasuku Honjo of Kyoto University, it’s in the 30 percents. If you offer the two in combination, there’s a 55% response.
With the monotherapies, which target one immune checkpoint, the response rate on kidney cancer is at about 30%. If you combine the two therapies, it’s probably going to be closer to 50% in both kidney and bladder cancer.
Researchers say that the immunotherapy breakthroughs are likely to come with the combination treatments. Do you agree?
Absolutely. Because cancer has certain vulnerabilities. In fighting it, we’ve got to think not just about the cancer cells but the whole tumor microenvironment. That’s a complicated thing. If you want to eliminate the tumor, you just have to take on multiple issues.
For example, there’s a trial underway right now for pancreatic cancer. It involves a chemotherapy drug, plus three different immunotherapy antibodies. They’ll probably add a little radiation to that. In the end, they’ll be giving patients five or six different agents. But with pancreatic cancer being pretty impervious to any single therapy, hitting it this way could get a response.
You have to remember that before ippy, the five-year survival rate after a diagnosis of metastatic melanoma was essentially zero. We started trials on the melanoma combination treatments five years ago. Half of these melanoma patients are alive today. The trick now is to find the combinations that can get us to 60, 70, 80%. It’s never going to be 100%, but it’s better than no hope at all.
Where did the underlying idea for immune checkpoint therapy come from?
It’s been around for a long time. The first person to propose using immunotherapy in a way close to what we’re doing now was Paul Ehrlich [one of the founders of modern immunology]. He worked out antibodies and structure and how they worked. When I was in Germany a while ago, I saw his 1906 data book, and there was a drawing of an antibody interacting with a cancer cell.
Listen, it’s been known for decades that cancer somehow thwarts the T cells — which are the attack cells of the immune system. So to get anywhere with a therapy, the question that had to be answered first was: How does it do that?
My team and other groups showed that with cancer, there were molecules on the surface of T cells that acted like an off switch, shutting down the immune response. They are called immune checkpoints. I wondered whether we could block the off switch that was shutting down the immune response and keep the T cells turned on.
What I did was find an antibody that inhibited the CTLA-4 immune checkpoint, shutting it off and allowing the T cells to go into the tumor and kill it. I termed the process immune checkpoint blockade.
Independently of my group, Tasuku Honjo of Kyoto University — I’d later share the Nobel Prize with him — found another immune checkpoint on T cells. His discovery was the PD-1 molecule that I mentioned earlier. The two are the basis of most of the currently approved immunotherapy drugs.
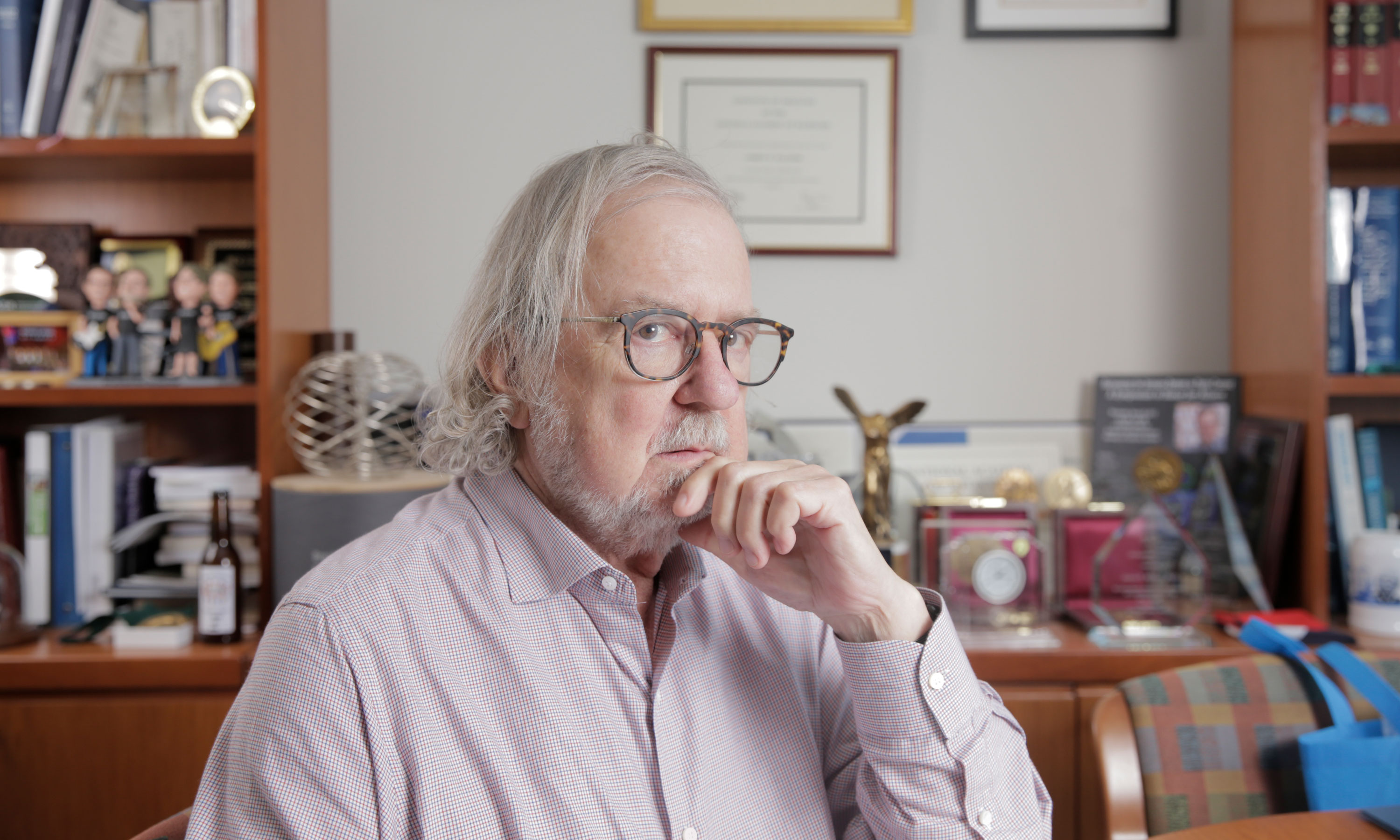
For many years, you were a kind of contrarian in the research world, an outsider. Have the Nobel and all the other prizes transformed you into an insider?
Well, maybe. Rather than me being outside, maybe everybody else has come inside to my house. [Laughs.]
What do you mean?
As we speak, there are something like 3,000 different immunotherapy trials underway.
The FDA has approved checkpoint inhibitor therapy for non-small cell lung cancer, small cell lung cancer, head and neck cancer, bladder cancer, Hodgkin lymphoma, some kind of diffuse large B-cell lymphoma, esophageal cancer, and some colorectal cancer that has defects to DNA damage. In fact, immunotherapy has been approved for any cancer type that has a defect in DNA damage repair called microsatellite instability.
The big pharmaceutical companies are now all players. Many, many early biotech firms are also trying to gain a presence. What you see, though, is that a lot of companies with patents on older, more conventional drugs are experimenting by combining them with checkpoints, just because they have the drugs. This is being done, in my opinion, without a lot of thought. A lot of them fail, but that information is usually lost because there’s no requirement for reporting. That’s still important information. So many combinations that are being tried are duplicative. It’s just a mess.
Are these trials being done on actual cancer patients?
Oh, yeah. They’re wasting patients. By that, I don’t just mean a large number of patients are not getting the treatments most likely to provide them benefit. Because we have a limited pool of patients, the most promising trials are not accruing sufficient patients fast enough to get these drugs to the clinic as quickly as we can.
Is that ethical?
I think it’s unethical. I think there shouldn’t be any trial where you don’t learn something.
Padmanee Sharma, who’s a clinical oncologist, and I have an operation here at MD Anderson called the Immunotherapy Platform. We’re currently involved in something like 117 different trials. We get tumor tissue from patients before and after treatment. We dissect it, looking for changes in cells, gene expression and structure. This can tell us something about what has happened.
If you are just looking for a clinical signal that a drug has worked or not, and that’s all you are doing, we might not learn anything.
A personal question. Padmanee Sharma is your second wife. One of the legends about you is that when you proposed to her, you said that the two of you ought to marry because nobody else could stand either of you.
What I meant was, nobody liked either one of us, because we were both too intense about T cells.
Now that you’re married, do you talk about T cells all day long?
On and off, yeah. It’s what we’re keen on. We also talk about music, and we have some fun every now and then. But not a day passes when we don’t talk about something relating to T cells, especially because of our work together on the Immunotherapy Platform.
Can we backtrack a little here? I’m wondering what drew you to doing scientific research in the first place. Were you one of those people who always knew this was what you wanted to do with your life?
No. When I started college, I knew I wanted to do some sort of biology — either that or be a doctor. My father had been a country doctor.

“To me, ‘interesting’ has always been the most important thing,” Allison said. “I can’t work on something that doesn’t fascinate me.”
Elizabeth Conley for Quanta Magazine
While at college — I was pre-med at the University of Texas — I saw that medical training involved filling your head full of stuff. Your job is to just pack your head with so many goddamn facts that if someone comes to you with a problem, you can make a diagnosis. And you’d better be right! Because if you’re wrong, you could hurt your patient.
Now as a research scientist, you’re supposed to be wrong. You have an idea about something that nobody understands and you’re trying to figure it out. And the only way you can do that is to have a hypothesis and do an experiment that says, “No, that’s not it.”
Why did you choose cancer research? Cancer is quite prevalent in your family. Your mother, father and brother died of it. Was that part of your motivation?
My motive was a complicated thing. I’m a basic scientist at heart. That’s what drove me. I can’t say I was driven to do cancer research. I got into science because I was interested in science.
You did your doctorate on the immune system?
No, it was on a cancer issue, but at the same time I did some immunology. I had this vague idea, “Maybe we can get the immune system to treat cancer.”
One time, just for the hell of it, I did an experiment. There’s an enzyme called asparaginase that’s still being used to induce remissions in kids with some kinds of leukemia. I had these mice I had cured with the enzyme, and I had another group of new mice I was giving tumors to. I thought, “Well, I’m just going to see if I can challenge these other guys that I’ve already cured with the asparaginase.”
I gave them the tumor. Well, it wouldn’t take! I gave ’em 100 times more of the tumor and it still wouldn’t take. They were immune. They rejected the tumor, whereas the untreated mice got sick and died unless I treated them with this enzyme.
I thought, “Wow, this is interesting. File it away.” To me, “interesting” has always been the most important thing. I can’t work on something that doesn’t fascinate me.
Back when you were doing your early research, immunology was not a particularly hot field. It was certainly not the place where a smart guy could make a reputation for himself. Given that, why go there?
You’re right. When I first came to Berkeley in the 1990s, for example, they were in the midst of trying to redefine modern biology, and certain very powerful people there did not even want there to be a department of immunology. They felt that immunology was not a real discipline because it didn’t deal with the static, fundamental processes of biology that apply to everything. To be a real biologist, they believed you needed to study things like how DNA replicates, how to make a protein, or how to make RNA. I thought they were silly.
Why silly?
Because there are certain key elements of immunology that immunologists pay attention to that people in other fields don’t. T cell biology, where the main principle is the recognition of the nonself, is an example. I wanted to know about how the immune system recognizes the nonself. How do you get to that? What regulates that? What are the cells and molecules involved? What helps you or stops you from recognizing the self? All these things are unique to the immune system.
Those were the questions that intrigued me. I eventually ended up identifying the T cell antigen receptor, which is the way T cells recognize anything at all.
So how did you battle against the conventional scientific wisdom?
After my postdoc at Scripps, I moved to what was then a new MD Anderson campus in Smithville, Texas. It was very new and very isolated. There were only six faculty members. I was the only immunologist there, so there was nobody to tell me I was wrong.
Sometimes, you just have to get away from everybody. I take some pride in the fact that I don’t think I read as many journal papers as other people. There was a period when I was working on the T cell receptor and I made a determined decision not to read a damn thing about T cell receptors because the papers were so confusing and contradictory. Some of the experiments weren’t even understandable.

The shelves of Allison’s office are filled with awards and other testaments to his celebrity as a scientist, including a bobblehead of his band, The Checkpoints.
Elizabeth Conley for Quanta Magazine
I’d think, “Either I’m too stupid to understand this, or nobody knows what they’re talking about. I’m just going to sit down and figure out something logical to me, making certain assumptions and predictions, and just do it.”
Why did you have enough faith in yourself to go it alone?
Because I could make certain minimal assumptions, based on a little bit of data. I know what science is. I know how to use it.
If somebody shows me that I’m wrong and has some data that’ll convince me of that, then I’ll admit I’m wrong. I mean, I’ve had to do that a few times. [Laughs.] Not too often, thank goodness.
When we met five years ago, you told me about one of the big moments in your life. In your off-hours, you’d been a country musician, and once, while you were still a postdoc, you got to play with Willie Nelson. Do you still see him?
I do. If he’s playing anywhere around here, his people call me. I played with them on Austin City Limits. It was a pretty big deal — there were 70,000 people there.
The last time I played with him, it was at his ranch. He had a party, and Mavis Staples was singing with him. So we did a gospel medley with Mavis Staples and Willie’s band, and me playing the harmonica. That was fun.
I once asked you whether you’d like your tombstone to read “Jim Allison, he played with Willie,” or “He cured cancer.” Since you can now say that you’ve done both, let me ask that again.
Either one. [Laughs.] I think I would like to just have something that says that the world is a better place because I was there.