What Happens When We Give Animals Our Diseases?

Maggie Chiang for Quanta Magazine
Introduction
When scientists think about the movement of microbes between animal species, we generally focus on “spillover” events: when pathogens move from animals to humans. But pathogen transmission isn’t a one-way street. Humans appear to have introduced SARS-CoV-2 — the virus that causes COVID-19 —into populations of wild deer, mink, captive gorillas, pet dogs and cats, and a variety of other species. This transfer of an infection from a human to an animal is colloquially referred to as a “spillback” of organisms. Such infections could have major consequences for the wild species, and for ours.
What illnesses can we spread to animals?
Viruses are perhaps the best-studied examples of spillback. For example, during the 2009 swine flu pandemic, caused by the H1N1 virus, a number of different animal species — including pigs and ferrets — were infected by humans. (We also likely spread influenza to pigs during the 1918 influenza pandemic, which was also caused by H1N1; the virus has evolved in swine populations globally ever since.) Early transmission of H1N1 to pigs in 2009 took place at agricultural fairs (a common site for influenza to spread across species), and ferret owners noticed infections early on during that pandemic. Urban wildlife was also affected, as H1N1-positive skunks were recently found in city parks in Vancouver, Canada.
Such well-documented spillbacks are likely only a small fraction of those that occur every year.
What about bacteria?
Bacterial spillbacks may be more common than viral ones, for several reasons. Bacteria can replicate in a broader range of species, since they often don’t require species-specific receptors on host cells, as viruses do. Bacteria may also be better at replicating on or in the mucous membranes, skin or intestinal tracts of a wider variety of animals, which would facilitate species jumps like spillover and spillback.
But because bacteria may be more likely than viruses to simply colonize their hosts — meaning they replicate in the host but don’t necessarily cause disease — bacterial transmission events are also easier to overlook.
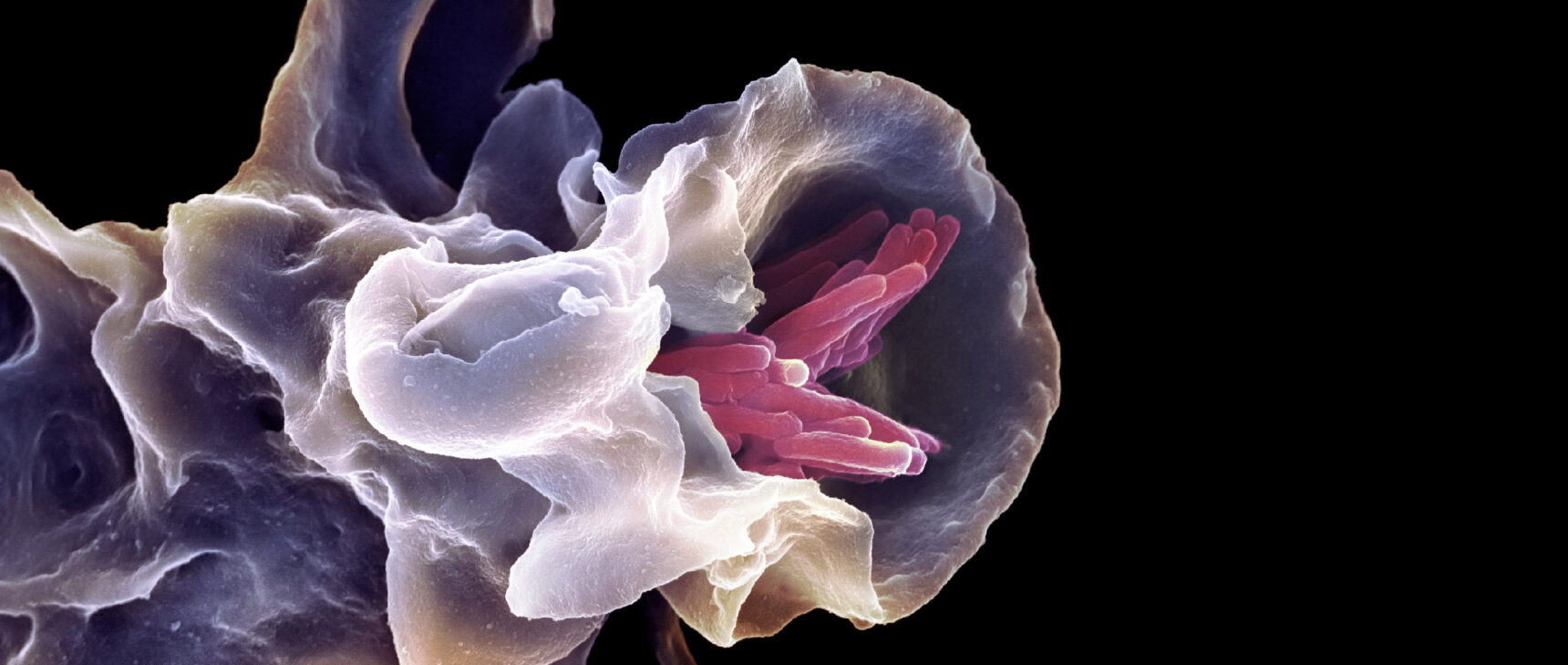
Numerous studies have identified spillback of Mycobacterium tuberculosis (the bacterium that causes tuberculosis) into animal populations. Tuberculosis-positive elephants have been reported since ancient times; it’s possible the bacterium travels back and forth between elephants and humans.
It is also likely that Hansen’s disease, or leprosy, first traveled from humans to armadillos. Now humans catch the disease by hunting or eating armadillo meat. The process is an example of secondary spillover, where humans are infected by a disease that they originally gave to a wild animal population.
What are the consequences of spillback for human health?
When infectious microbes repeatedly replicate in different animal species, their evolutionary trajectory may be different from one species to another, potentially creating novel variants that could evade immunity if reintroduced into humans.
Consider the case of Staphylococcus aureus, a bacterium that can cause diseases ranging from minor skin infections to pneumonia and drug-resistant staph infections. S. aureus has a wide host range, thriving in mammals from dolphins to mountain goats, as well as in many species of fish and birds. As with the armadillos, multiple studies have used genomic sequencing to reconstruct species jumps from humans to animals and back to humans. But with S. aureus, there’s an unfortunate twist: The microbes continue to evolve and gain antibiotic resistance within the animals. When the disease returns to humans through secondary spillover, the disease is harder to treat.
Similarly, human types of E. coli may follow a similar cycle of bidirectional transmission between pets and their owners. A highly antibiotic-resistant strain found commonly in human hospitals, termed O25:H4-ST131, was identified in a European-wide study of companion animals that had urinary tract infections, wound infections and diarrhea.
In addition, we may have already seen secondary spillover of SARS-CoV-2. While many scientists believe the source of the omicron variant that emerged in late 2021 was likely an immunocompromised person with a chronic infection, several of omicron’s mutations have been previously seen in rodent-adapted lineages of coronaviruses. It could be that a population of rodents, such as urban rats, was exposed to human viruses via virus-laden sewage, allowing the virus to evolve into the omicron variant and spread back into the human population via rat contact.
What about animal health?
Spillback events can also harm fragile wildlife populations. A recent publication includes a scenario where the animal target of the spillback is not a good transmitter, but instead is a dead-end host species with the potential for significant mortality. Spillback into these populations could be disastrous for the affected species, possibly even putting it at risk of extinction.
Because scientists were already monitoring critically endangered mountain gorillas in central Africa, they recognized a spillback of human metapneumovirus (HMPV) infection into that population in 2009. HMPV is a respiratory pathogen that causes a flu-like infection in humans, and researchers spotted similar symptoms in a group of mountain gorillas in a protected park in Rwanda. HMPV was eventually detected in tissues from a sick animal that died. Though it’s not clear how the apes were infected, the strain of HMPV matched samples from humans in South Africa, and ecotourism was common in the park. Strains of HPMV and human respiratory syncytial virus (HRSV) were also found in chimpanzees that had died from respiratory infections in Côte d’Ivoire in 2008.
Researchers later investigated the problem of spillback in great ape populations in Africa in detail. They found that introduced infections could have devastating effects on the population. Scientists have suggested that tourists in nearby areas keep their distance from the apes, wear masks and stay fully vaccinated against a large number of diseases. Unfortunately, we don’t know whether this will be enough to protect the ape populations.
Can other pathogens cause a spillback event?
Parasites and fungi can also jump from humans to animals. But because these pathogens are typically less deadly than bacteria and viruses, they are generally under-studied in human populations. As a result, there are fewer documented spillback events for these microbes.
Parasite spillback in particular is tough to track. Parasites have complex life cycles, making cross-species transmission less likely, and many of them have a stable presence in the environment, so it is not always clear if humans are the source of infection. But a few spillback events have been suggested, based on indirect evidence. We suspect humans have passed Giardia duodenalis (a gastrointestinal parasite that can cause diarrhea and cramping) to red colobus monkeys in western Uganda, based on similar molecular types found in both species and a high level of Giardia duodenalis infection reported in nearby villages.
On the fungal side, the pathogen Candida albicans can cause several symptoms in humans, including vaginal, urinary tract, skin and oral infections. One study found that while human types of the pathogen were rare in wild animals, they were present; the authors suggested that human-to-wildlife transmission could occur via an environment contaminated with “by-products of human life,” such as diapers and leftover food products. Human strains were also detected in pets.
How can we identify spillback?
Discovering spillback events is a matter of money and luck. Spillover into the human population is generally recognized only during routine surveillance — when scientists are looking closely for novel pathogens — or when the introduced pathogens cause a cluster of infections, as with HIV, SARS-CoV-1, SARS-CoV-2, Ebola and others. We have very few surveillance programs looking for human pathogens in animal populations, so spillback events are easy to miss.
When we do spot spillback, it’s frequently in animals that we monitor closely: pets, livestock, captive animals and occasionally endangered species under close observation. These are the animals with the most intense human contact, so they’re most likely to be infected with our microbes.
Furthermore, it’s hard to get concrete evidence of many spillbacks. Often the presence of a human-typical pathogen in an animal species suggests transmission from a person to the animal, but because many pathogens remain stable in the environment, the two species may never be in close contact before transmission occurs. And even if molecular types match, that doesn’t always confirm the direction of transmission (human to animal or the reverse). Both species could even have been infected from an unknown third source.
If we want to minimize disease, we need to better understand the organisms in our shared ecosystems. While it’s understandable that our focus is mostly on humans, that focus may ultimately prove costly both to us and to those who share our planet.