Why South Asia’s COVID-19 Numbers Are So Low (For Now)

At a mobile testing center in New Delhi, India, people wear protective face masks as they wait to be tested for exposure to COVID-19, the pandemic coronavirus.
Reuters/Adnan Abidi
Introduction
With 1.94 billion people, South Asia is home to almost exactly one-quarter of the world’s population. The region, comprising eight countries — Afghanistan, India, Pakistan, Bhutan, the Maldives, Bangladesh, Sri Lanka and Nepal — is extremely poor, densely populated and geographically close to China, where the SARS-CoV-2 virus originated. The COVID-19 pandemic was expected to be a “perfect storm” for the region. However, as of June 22, South Asia had reported a total of only 765,082 confirmed cases and 19,431 deaths, accounting for just 8.5% of global infections and 4.1% of world fatalities — even as the numbers in some South Asian countries have spiked drastically in the past few weeks.
Many reasons have been offered over the past few months as to why South Asia might be an outlier in the pandemic: its tropical climate, protection offered by a tuberculosis vaccine called Bacillus Calmette-Guérin (BCG), exposure to malaria, and a weaker strain of the virus in the Indian subcontinent. However, Quanta spoke to 15 global health and infectious disease experts, researchers and epidemiologists, all of whom warned that there is little scientific evidence to back most of these claims.
“There is currently no data to suggest better immunity among South Asian populations, no reason to believe the potentially small benefit of hot, humid weather will even be visible against a backdrop of a nearly 100%-susceptible population,” said Jessie Abbate, an infectious disease and epidemiology research scientist with the French Laboratory for Translational Research on HIV and Infectious Diseases and the geospatial informatics company Geomatys. “There is no evidence of any functional mutations resulting in different ‘strains’ of the virus anywhere (let alone strains with different rates of virulence), and a recent study has shown there to be no correlation between BCG vaccination and COVID-19 susceptibility.”
It is therefore very unlikely that the novel coronavirus will have any less of an effect on South Asian populations. On the contrary, Abbate said, high densities in overcrowded South Asian cities pose a huge problem for control measures that rely on social distancing.
To understand what is behind South Asia’s low COVID-19 numbers to date, consider Afghanistan. Its health minister estimated on March 24 that 80% of the war-torn nation’s population might be infected with COVID-19 within five months — resulting in more than 25 million cases with possibly 110,000 fatalities. This would represent a mortality rate of 0.4%, significantly lower than the 1.4% infection fatality rate observed in New York City, for example. As of June 22, however, only 29,143 confirmed cases and 598 deaths had been reported.
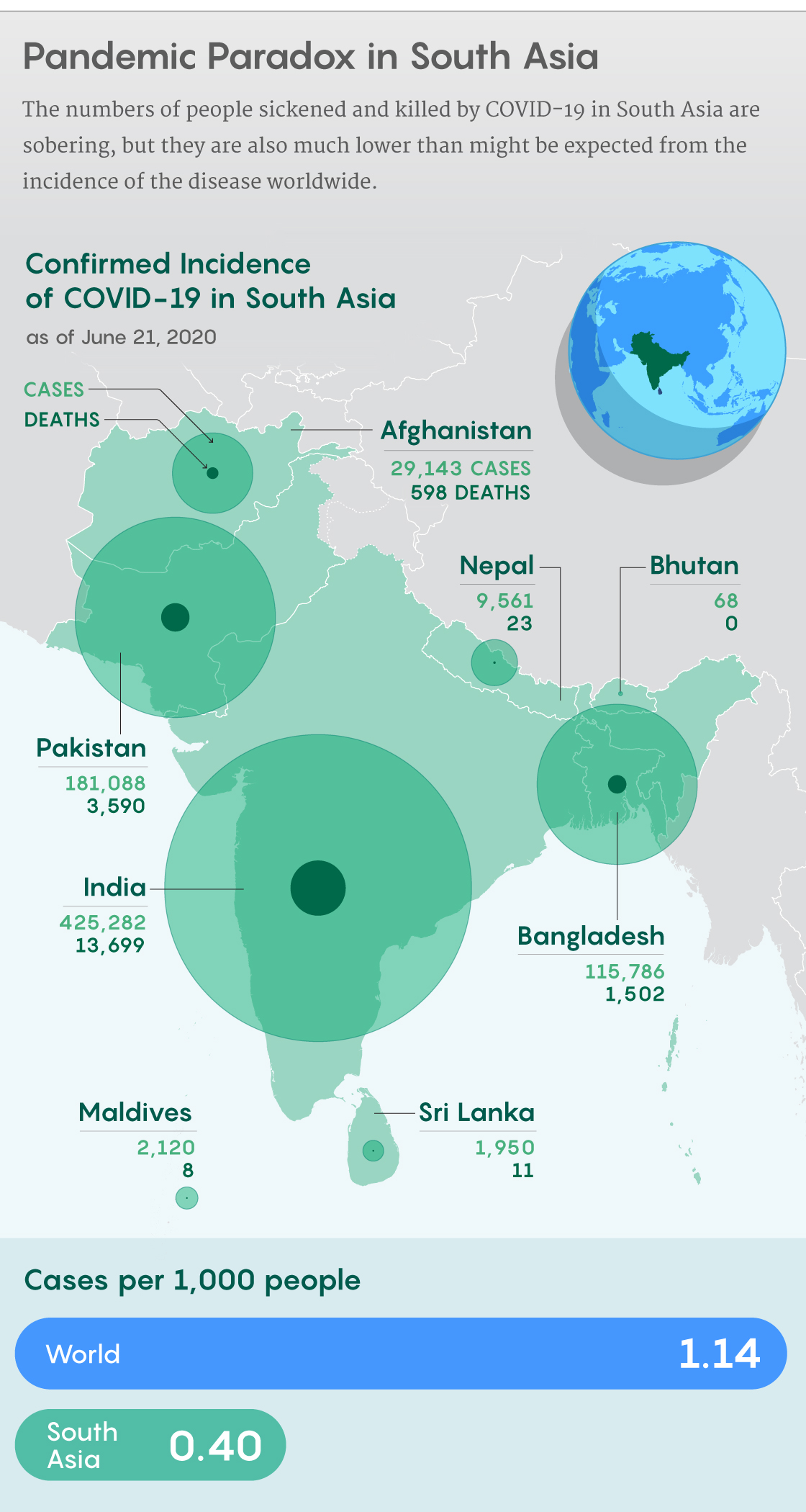
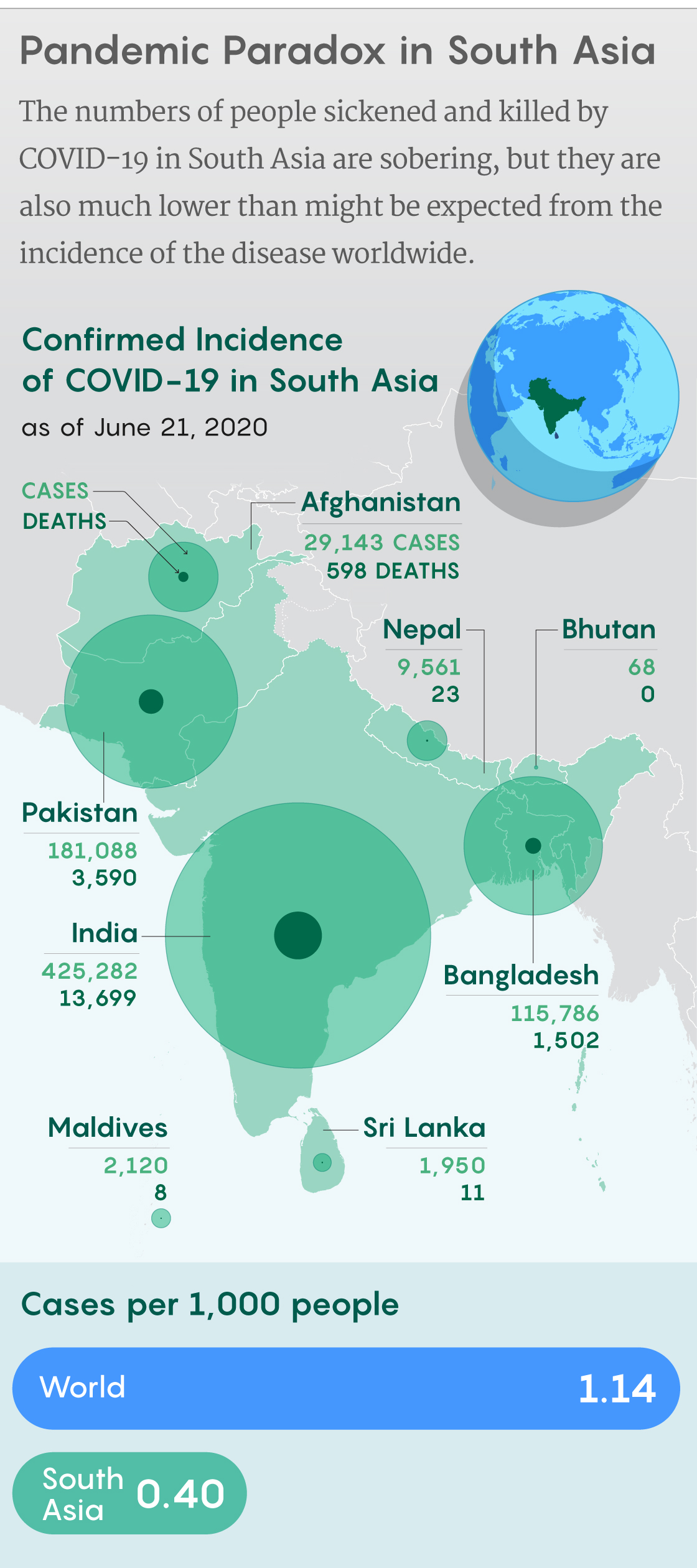
Samuel Velasco/Quanta Magazine;
sources: Our World in Data, Johns Hopkins Corona Resource Center, World Bank
The low numbers do not depict the real situation, according to experts. Nicholas Bishop, a Kabul-based emergency response officer with the United Nations International Organization for Migration (IOM), said that based on extrapolations of testing data, the true number of COVID-19 cases in Afghanistan is in the millions, “as community-level transmission is significant across all 34 provinces.” Poor testing rates, inadequate health infrastructure and violent conflict, among other factors, have masked the actual extent of infection.
“Afghanistan is presently only testing 646 persons per million,” said Bishop. “This is one of the lowest rates in the world and explains why the total official confirmed-case count remains low. Testing is constrained by limited availability of tests and related materials such as RNA extraction kits, reagents, qualified lab technicians and rapid-response sample collection teams, who are further limited by escalating levels of conflict” — a reference to the more than 4,500 attacks in the nation since the beginning of the year by non-state armed groups.
South Asia appears to be an anomaly in the pandemic due to inefficient epidemiological data, according to experts. Epidemiological research has been fast-tracked because of the urgent need for answers about the swiftly moving COVID-19 pandemic, and that urgency has led to a deluge of data — but it ranges from statistically powered robust analyses to poorly designed studies fraught with methodological and ethical issues, said Seema Yasmin, an epidemiologist and director of the Stanford Health Communication Initiative.
“The conclusions from these studies are often made not by the scientists but by the public, who is presented with sometimes misleading headlines drawn from published data,” said Yasmin. “This can affect the public’s trust in science and the scientific process and has the potential to hamper public health efforts.”
The Hypotheses
Perhaps the most popular justification for the relatively low number of COVID-19 infections and deaths reported in South Asia is the region’s warm, humid climate. In April, for instance, the Trump administration announced findings from a new study that claimed the novel coronavirus loses potency with increased sunlight, heat and humidity. Experts object, however, that this is a correlation without a mechanism. The World Health Organization has also cautioned that high temperatures cannot prevent the COVID-19 disease.
Vikram Patel, a global health professor at Harvard Medical School, dismissed the influence of weather on the novel pathogen. “Certainly the spread of the virus in Mumbai, Chennai and New Delhi in the midst of peak summer heat and humidity pretty much settles the issue of whether climate neutralizes the virus,” he said.
“I cannot posit a reasonable mechanism to explain a climate link,” said Sadie Ryan, a global health expert and medical geographer at the University of Florida. “In broad senses, we may see seasonal associations during the year when people aggregate, which would increase transmission opportunities — for example, school terms are often implicated in epidemics of directly transmitted diseases like flu.” COVID-19 infection trends might vary with the climate in that way, but they would be independent of it.
Another hypothesis involves the BCG vaccine, a century-old inoculation against tuberculosis that has been touted as a “flak-jacket” and a “game-changer” against the novel coronavirus. In South Asian countries, where the vaccine has been used universally for decades, it’s been suggested that people are less susceptible to COVID-19 morbidity and mortality owing to the immunity offered by BCG.
In an April review of the evidence, the WHO examined three studies still undergoing peer review in which the authors observed that countries routinely using the BCG vaccine had less incidence of COVID-19. The WHO concluded that “such ecological studies are prone to significant bias from many confounders,” including differences in national demographics, testing rates for COVID-19 infections, and the stage of the pandemic in each country.
Arvind Mathur, a WHO representative to the Maldives, pointed to that scientific review and its conclusion that there is no evidence that the vaccine would be protective in the pandemic. “Currently, in the absence of any such evidence, WHO does not recommend BCG vaccination [for] the prevention of COVID-19,” he said.
Wafaa El-Sadr, a professor of epidemiology and medicine and the director of ICAP at Columbia University, agreed. “This is only a hypothesis, yet to be proven,” she said.

Sri Lankan health officials arrive in a residential neighborhood in Columbo to collect swab specimen from the suspected COVID-19 cases.
The third argument that positions the Indian subcontinent as an anomaly in the COVID-19 pandemic is that a weaker strain of the virus is abroad in parts of the region. On Twitter on March 24, the noted Indian parliamentarian Subramanian Swamy wrote that he had heard the COVID-19 strain in India was a “less virulent mutation,” which could be defeated by “our body’s natural defensive mechanism.” Others made similar assertions, all of which were subsequently dismissed by virologists as baseless.
The virus is changing, and local variants do emerge, according to Raul Rabadan, the director of the Program for Mathematical Genomics at Columbia and author of the forthcoming book Understanding Coronavirus (Cambridge University Press). “The key question, however, is if any of these differences is functional or just a passenger mutation carried along with the virus,” he said. “There is no convincing evidence that any mutation is associated with infection or severity.”
Rabadan also dismissed the proposition that the relatively low number of cases in South Asia can be attributed to the exposure of a large part of its population to anti-malaria drugs — in particular the drug hydroxychloroquine. President Trump touted the drug as a “game changer” in the fight against coronavirus in early April, but on June 15, the Food and Drug Administration revoked its emergency use authorization to treat COVID-19. Basing the move on results from a large, randomized clinical trial in hospitalized patients, the FDA stated that the anti-malaria drug “showed no benefit for decreasing the likelihood of death or speeding recovery.”
“I have not seen any convincing evidence linking malaria exposure with severity of COVID-19,” said Rabadan. “There is a lot of speculation but not convincing evidence for many of these hypotheses.”
The Struggle for Reliable Data
Although COVID-19 has put a spotlight on epidemiological research, the biggest problem, scientists say, is finding reliable data. It is difficult for epidemiologists to gather data during a pandemic like COVID-19, particularly when the information is originating from a multitude of disparate sources. Scientists are performing different tests, using different case definitions or reporting methods, and using different time intervals across different geographical areas. These inconsistencies make it hard to pool or compare data, Abbate says, even when the funds and infrastructure are in place for the research. It also takes time and effort to develop data-sharing mechanisms such as systems that can store test results anonymously without hindering their accessibility.

Outside a government hospital in the city of Srinigar in India, people queueing up for service stand in special designated places to maintain a safer social distance and limit the spread of COVID-19.
“Most health systems are not set up for wide-scale rapid anonymization of testing numbers and results, leading to inconsistencies among studies,” said Abbate. “Even the number of deaths is calculated differently between locations, with some including only those who die in hospital, or only those who were confirmed to have died from the virus. This is, of course, nothing new, but it has highlighted the need for international standards on ethics and reporting mechanisms that are flexible but responsive.”
Another issue is the reliance on older studies of other coronaviruses, to which some scientists are turning for quick answers and correlations. For instance, the claim that tropical weather reduces the potency of SARS-CoV-2 is partly based on studies of other coronaviruses that seemingly peaked in winter and disappeared in spring. These observations, however, might not apply to the novel pathogen.
“During this epidemic, time is of the essence,” said Caroline Genco, a professor of immunology and vice provost for research at Tufts University School of Medicine. “We must avoid a false sense of security and keep in mind that while existing data on this and other coronaviruses provide valid bases for theories that ought to be tested, they should not be acted upon until further research is performed if doing so would increase population and individual risks.”
More than 29,400 research papers on SARS-CoV-2 and the COVID-19 disease have appeared since January 2020. However, many of these papers are uploaded to open archives as preprints, without peer review. Preprints enable quick data sharing between scientists and researchers, but they also allow questionable literature to enter public discourse without the necessary scrutiny.
“Preprints pose an issue as the findings can make their way to news stories without the requisite caveats that the research has not yet been peer-reviewed and may never make it through the peer-review process,” Yasmin said. “This has allowed less than robust science to enter the public arena and further challenges the public health response and public understanding of the situation.”
“Recently, questionable papers, which have made it through the peer-review process, have come to light,” said Genco. “There are concerns that the expedited review for COVID-19 papers may enhance this problem” or add to the confusion, she said.
Acting on incomplete or misleading data that positions South Asia as an outlier in the pandemic could prove fatal, scientists warn. “It is exciting and encouraging to see researchers investigating such diverse avenues,” Genco said. “But until definitive studies have been performed, governments should not assume such factors provide any protection. It would be irresponsible to act on such theories without proper support,” because the consequences could be a potentially catastrophic loss of life.
The More Plausible Explanations
According to a recent paper co-authored by Patel in The Lancet, the world’s richest countries accounted for more than 90% of all reported COVID-19 deaths by early May. Demographic data from the Centers for Disease Control and Prevention reveal that age is one of the biggest risk factors for the disease. In the U.S., patients 65 years and older have accounted for 80% of deaths from the novel coronavirus. The Indian subcontinent, meanwhile, has a relatively young population, with a median age of 27.6 years. This, experts say, is one of the more reasonable explanations for the relatively low number of COVID-19 infections and fatalities in South Asia.
“If you consider Europe, [the] majority of the COVID-19 deaths were among older citizens, many of them living in nursing homes or institutionalized care facilities,” said Adnan Khan, a public health and infectious disease researcher based in Islamabad. In contrast, very few of the elderly in the Indian subcontinent are in nursing homes. Khan suggests that because these elderly people instead live at home with their families, they are less vulnerable. According to an analysis published on June 16 by The Wall Street Journal, deaths among staff and residents of senior care facilities account for 40% of the overall COVID-19 deaths in the U.S.

An elderly man in Delhi looks out from his balcony during the government lockdown. Because parents and grandparents in South Asia tend to live with their adult children, they may be protected from the outbreaks that have been so deadly in many elder care facilities elsewhere.
In mid-March, as the pandemic was gaining momentum across the world, the WHO called on all countries to ramp up their testing capabilities as a way to break the chains of COVID-19 transmission. “You cannot fight a fire blindfolded,” said Tedros Adhanom Ghebreyesus, the organization’s director general, during the press briefing. “And we cannot stop this pandemic if we don’t know who is infected. We have a simple message for all countries: Test, test, test.”
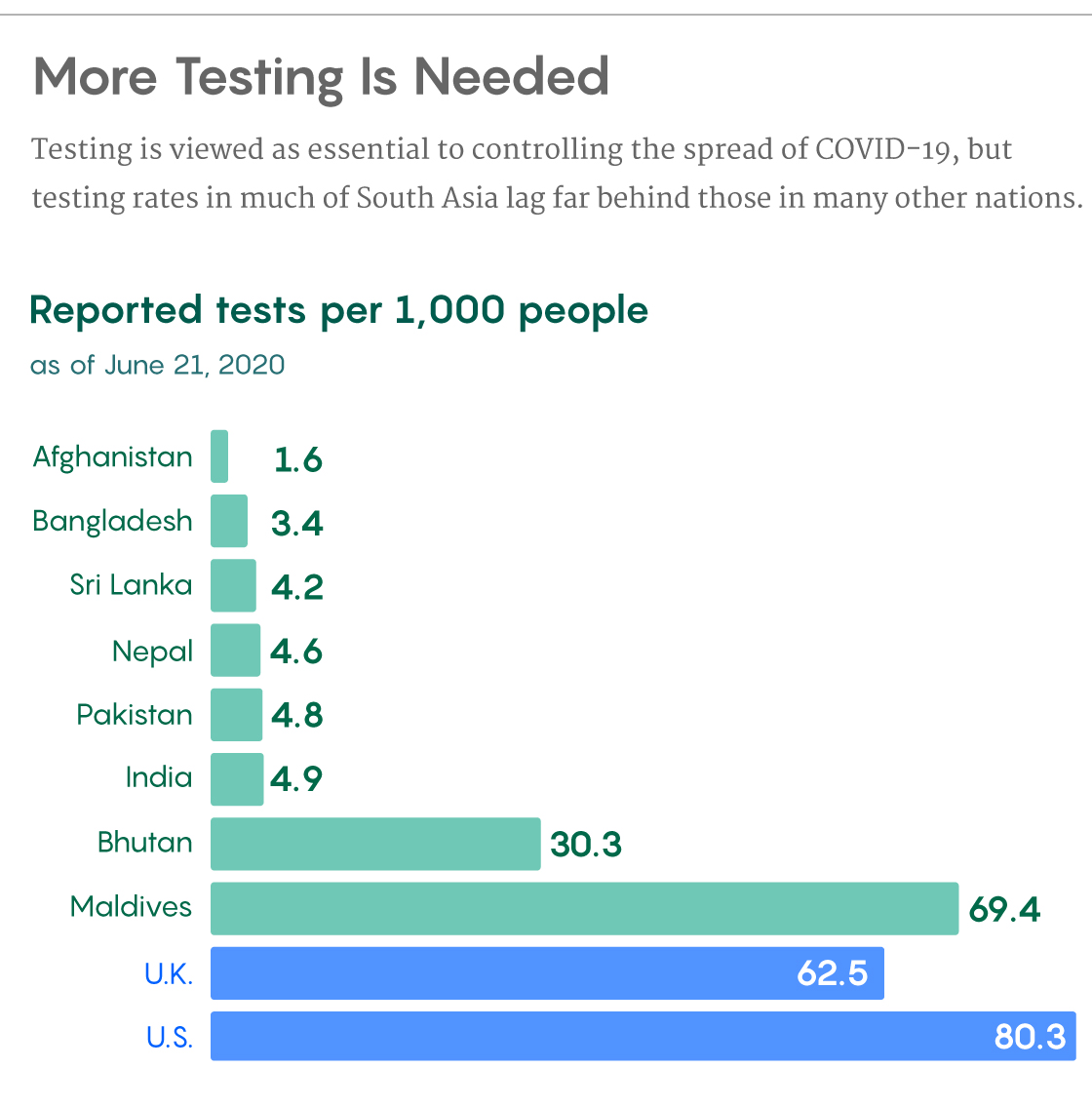
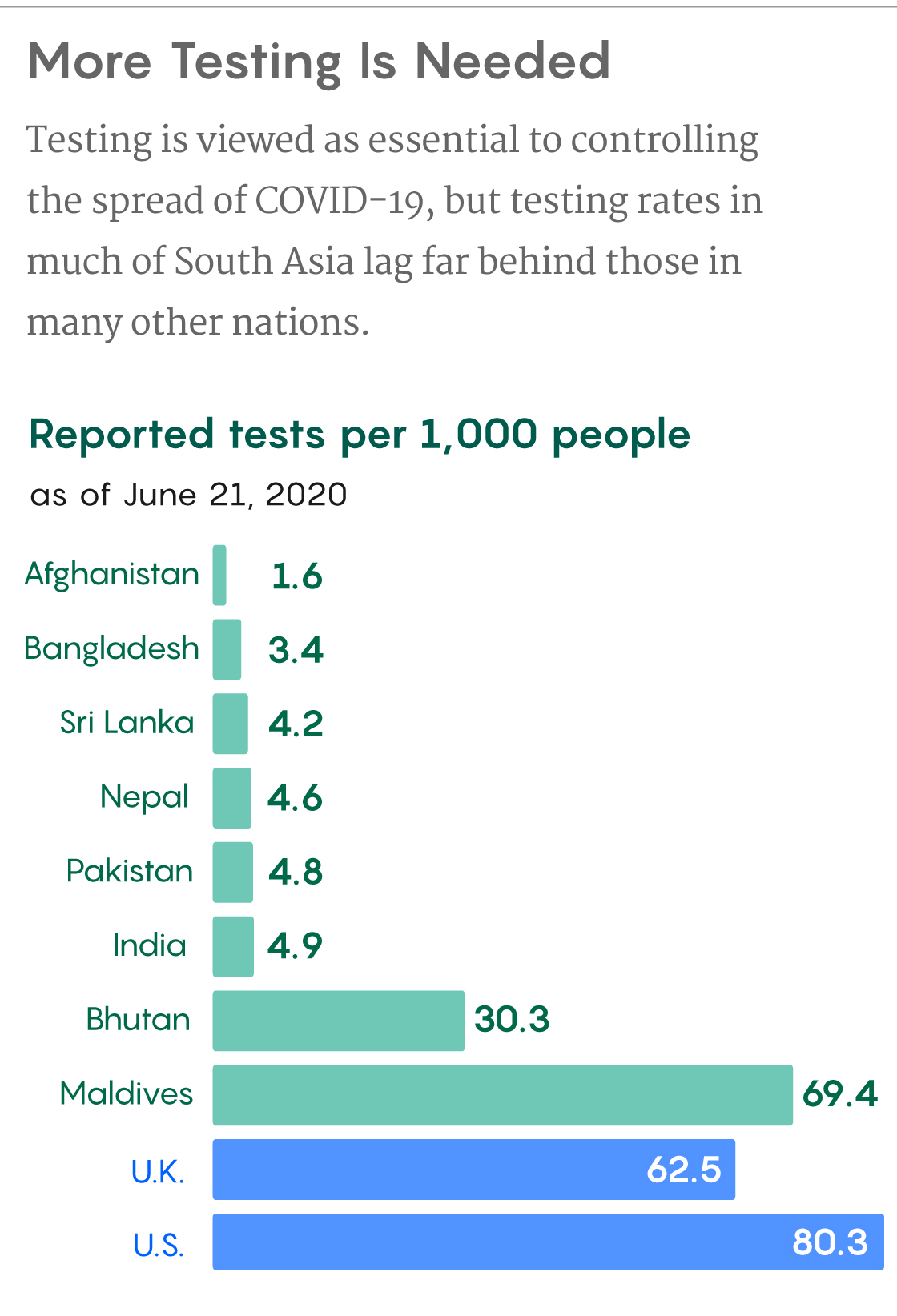
Yet most South Asian countries still have some of the lowest testing rates in the world. As of June 21, India performed 4.9 tests per 1,000 people, as opposed to 75.7 tests per 1,000 in the U.S., 70.4 in Spain, 62.5 in the U.K. and 116.5 in Russia. The numbers are also bleak for other major countries in the Indian subcontinent: 4.9 tests per 1,000 in Pakistan, 4.6 in Nepal and 3.4 in Bangladesh.
In Afghanistan, meanwhile, the lack of testing is pushing the country toward a humanitarian disaster. According to Bishop, because populations living in areas controlled by non-state armed groups have extremely limited access to testing, coherent statistical information about the extent of the pandemic there is unavailable.
Bangladesh, with possibly the lowest testing rate in South Asia, ramped up its testing capabilities in May, but the present capacity is still insufficient, said Salim Uzzaman, an infectious disease epidemiologist with the Institute of Epidemiology, Disease Control and Research in Dhaka. “Good testing capacity is the key to understand the total number of cases,” he said. But because the epidemiologists lack antibody testing kits that are sufficiently sensitive and specific, they cannot perform the kind of “community surveillance” that would help them understand the spread of the disease.
Bhutan and the Maldives seem to be exceptions to the poor testing record of South Asian countries. Bhutan, with more than 30.29 tests per 1,000 people, and the Maldives, with 69.36 tests per 1,000, fare much better than other countries in the region. Moreover, Mathur said, the testing, surveillance and tracing strategy is “so robust” in the island nation that every positive test result leads to all of the patient’s contacts being tested as well. Still, Bhutan and the Maldives, with populations of about 771,600 and 540,500 respectively, account for just 0.068% of the total South Asian population.
Another reason for the relatively low number of COVID-19 cases and fatalities in South Asia, experts say, could be poor documentation of deaths. According to a 2018 UNICEF report, only 60% of South Asian children under five years of age are registered and have a birth certificate, and deaths are registered at an even lower rate in many countries in the region. The report showed that Bangladesh missed recording over 90% of its deaths in 2014, while India missed 29%, Nepal missed 25%, Bhutan missed 19%, and the Maldives missed just under 10%. Data for Afghanistan and Pakistan were not available in the report, but Bishop said that Afghanistan does not have an official death registry. Pakistan, meanwhile, had almost no death registration mechanisms until a decade ago.
Samuel Velasco/Quanta Magazine;
sources: Our World in Data, Johns Hopkins Corona Resource Center, World Bank
Death counts are important because tracking the infection fatality rate is one of the more reliable ways to gauge the impact of COVID-19, said Prabhat Jha, an epidemiologist with the Dalla Lana School of Public Health at the University of Toronto. To determine the denominator for that calculation, “we need national random samples with a large sample size with antibody assays to determine who has been infected,” he said. However, he added, eight of 10 million overall deaths in India occur at home, and even registered deaths have no useful information on cause.
“The Indian Registrar General needs to do an updated survey of deaths,” said Jha. For COVID-19, the governments of India and other nations should be releasing anonymized data on cases daily and on deaths weekly, the way Singapore does, he said. “These data are part of the response.”
Experts believe that the COVID-19 numbers in South Asia are relatively low so far because early and stringent lockdowns delayed the disease’s peak in the region. For example, said Pratik Khanal, a research member of the Nepal Public Health Association, a nationwide lockdown was imposed in Nepal on March 24, a day after the second case was detected and it was kept in place until June 14.
“The lockdown restricted the movement of people, led to the closure of domestic and international flights and closure of nonemergency services,” Khanal said. This bought time for the government to expand testing facilities from just one to 19 across the country, to trace the contacts of infected people, and to prepare health facilities to handle the uptick in cases. Nevertheless, Khanal continued, Nepal still lacks the necessary infrastructure to handle the epidemic, and the government should “coordinate with private sector hospitals for expansion of testing facilities and hospitalization of COVID-19 cases.”
In India and other South Asian countries, where the lockdown restrictions are now being eased, the number of COVID-19 infections and deaths is rocketing. “India shut down the entire country, which even China didn’t, so that clearly had a role in stopping the rate of transmission of the virus,” said Thomas Abraham, a specialist on disease risk communication at the University of Hong Kong and a former consultant for the WHO. He acknowledges that India’s lockdown, which started on March 25, was “unsustainable” and imposed “an enormous human cost.” But its check on the spread of COVID-19 is now over. “So now the virus is spreading once more, and it’s going for a wider geographic area.”
Uzzaman agreed, saying that Bangladesh’s early national lockdown beginning on March 26 reduced the number of cases and flattened the curve of the disease. But even then, he said, “the challenge remains as for any other country to handle the full onslaught of the pandemic.”
The Sri Lankan government appears confident about handling its share of the pandemic, said Gulbin Sultana, a research analyst with the New Delhi-based South Asia Center at the Manohar Parrikar Institute for Defense Studies and Analyses. However, the country may not have enough quarantine facilities, ventilators or trained medical professionals to care for patients as infections rise.
“We will know the real impact of the virus in the Indian subcontinent in the coming weeks,” she said.
The Road Ahead
Mathur emphasizes that there is no South Asian exception in the COVID-19 pandemic. As of June 22, the world has reported over 9 million COVID-19 infections globally and over 469,000 deaths from more than 200 countries, irrespective of cold, heat, humidity and other weather conditions. “I can confidently say that a person of any age, genetic makeup, race, religion or ethnicity can get the infection with this virus. It’s important to understand that it could be transmitted to any person,” he said.
The prospect of accelerating rates of transmission in most South Asian countries is especially daunting because spending on public health there is worrisomely low. According to World Bank data, Bangladesh spent just 2.27% of its gross domestic product (GDP) on public health in 2017, as opposed to 17.06% in the U.S., 10.4% in Austria, 8.84% in Italy and 9.47% in Brazil. The numbers are similarly alarming for most other countries in the Indian subcontinent: 2.9% in Pakistan, 3.19% in Bhutan and 3.53% in India. The Maldives and Afghanistan fared better with 9.03% and 11.78% respectively.
Those numbers, however, fail to capture the magnitude of the mounting crisis. In 2018, the GDP per capita for the whole of South Asia was only about $1,900, compared with $35,600 for the European Union and $62,900 for the U.S. South Asian nations can therefore spend only a fraction of what wealthier nations can on each patient.
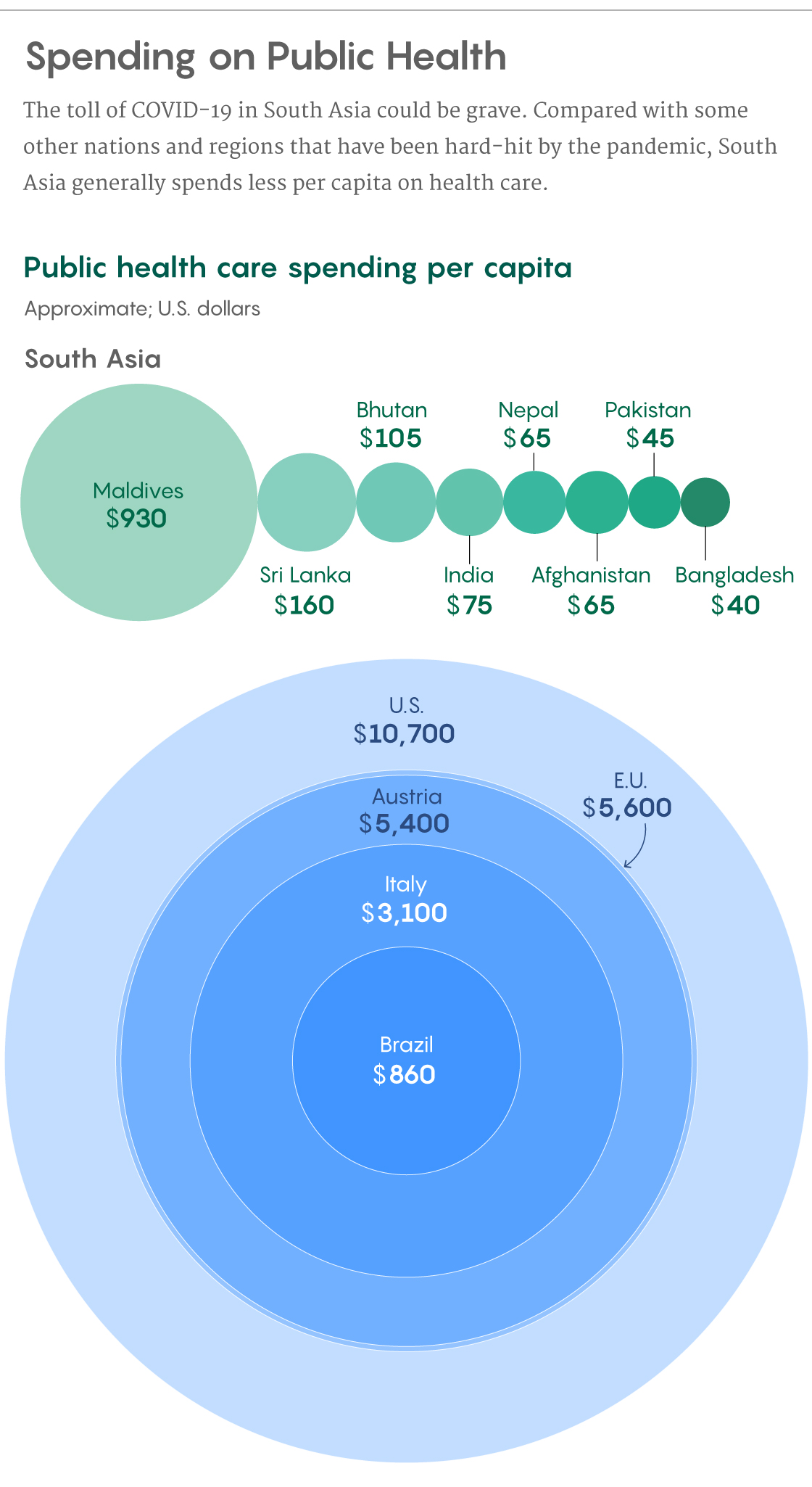
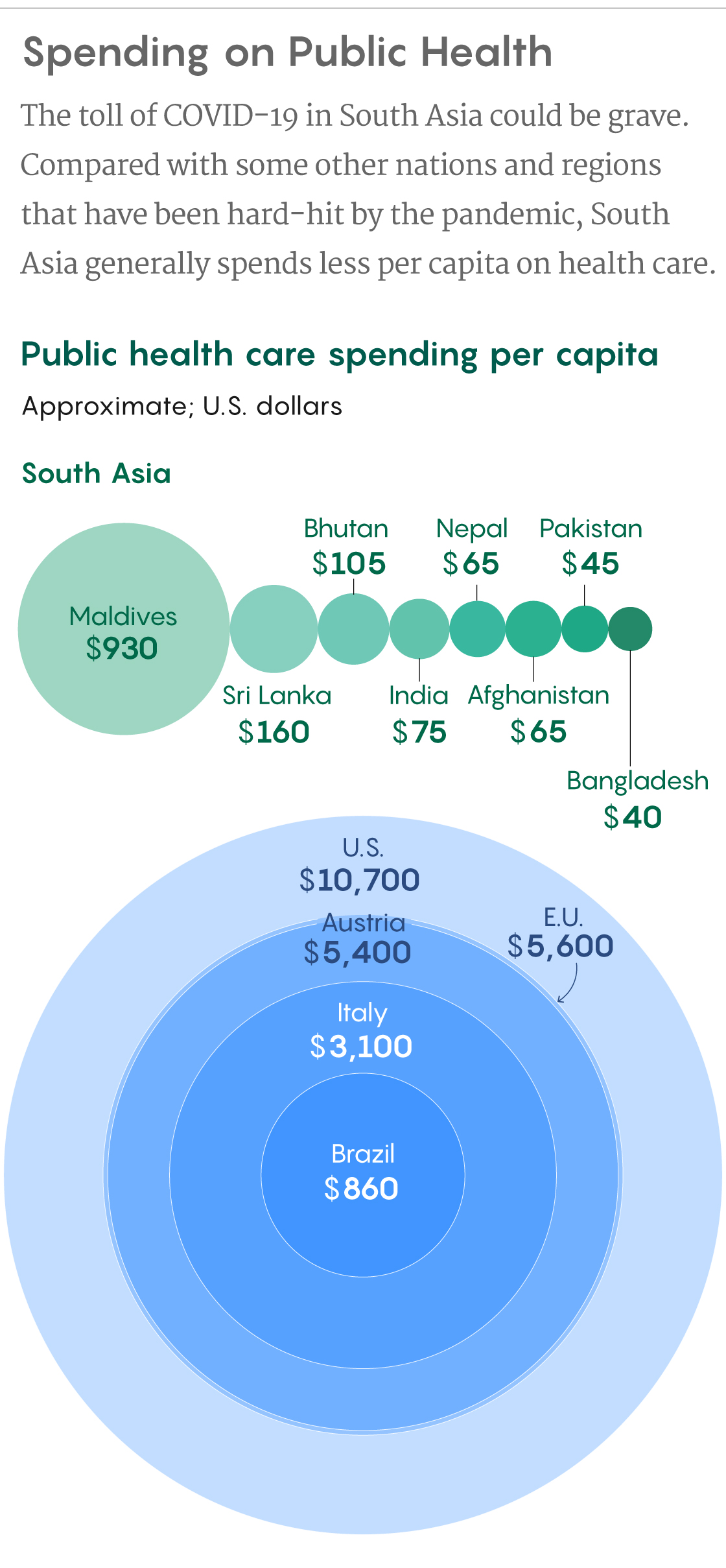
Samuel Velasco/Quanta Magazine;
sources: Our World in Data, Johns Hopkins Corona Resource Center, World Bank
Because of that limited health spending, experts warn, most South Asian countries have crumbling health infrastructures that are ill equipped to handle the COVID-19 onslaught. Bangladesh, India, Pakistan, Nepal and Afghanistan do not have even one hospital bed per 1,000 people, while the numbers stand at only 4.3 hospital beds per 1,000 people in the Maldives, 3.6 beds per 1,000 in Sri Lanka and 1.7 beds per 1,000 in Bhutan. The numbers of available physicians are even more dire: Pakistan and Sri Lanka have one physician per 1,000 people and the Maldives has four. The remaining five countries do not have even a single physician per 1,000 people.
As South Asian countries ease their lockdown restrictions, many are witnessing a drastic rise in COVID-19 infections. For instance, the national lockdowns in Pakistan and Bangladesh were lifted on May 9 and May 30 respectively, and they loosened in India in early June. All three nations recently reported their highest single-day spikes in COVID-19 cases.
Experts warn that in South Asia, the pandemic is likely to develop along a trajectory similar to that seen in other affected nations. Abraham said that there might have been a lag in terms of the pace of virus transmission in South Asia, but in three to four years, “we will find that there’s pretty much uniformity across the globe.”
With COVID-19 infections and fatalities now on the increase, “South Asia should focus on health-system readiness to prevent, control and manage the COVID infections, as the socioeconomic consequences of the disease on the countries will be lethal,” Khanal said.
To that end, there is also a need for better epidemiological data, experts said. Abbate said that science always has room for hypotheses about atypical patterns in the spread of the coronavirus, but investigating the hypotheses before determining the actual extent of infection and its severity patterns — through adequate testing and reporting of cases and outcomes — “is a waste of time, effort and resources.”
Jha agreed and added, “We need not just love in the time of cholera, but data.”