New Genomic Study of Placenta Finds Deep Links to Cancer
New work shows that the human placenta is a mosaic of cells with different genotypes. This heterogeneity may be a consequence of the organ’s protective function.
Samuel Velasco/Quanta Magazine
Introduction
In 2008, while the medical resident Sam Behjati was doing his usual rounds in a hospital maternity ward, a colleague urgently pulled him into a patient’s room, where he saw a mother beaming with joy and swaddling a perfectly healthy newborn. Behjati’s jaw dropped. Only a few months earlier, doctors had given this mother the devastating news that a routine prenatal test — which had analyzed a sample from her placenta — showed that her baby had an extra copy of chromosome 13, a condition typically fatal for newborns. Yet postnatal tests showed that the baby had 23 normal pairs of chromosomes. “I walked away from the room thinking, ‘How can that possibly be?’” said Behjati, who is now a geneticist at the Wellcome Sanger Institute.
Behjati had uncovered a case of confined placental mosaicism (CPM), a condition in which patches of the placenta have genomes that don’t match up with that of the fetus — a strange phenomenon given that the placenta and fetus derive from the same fertilized egg. Scientists have known about CPM for decades, and they estimated that it occurs in less than 2% of pregnancies.
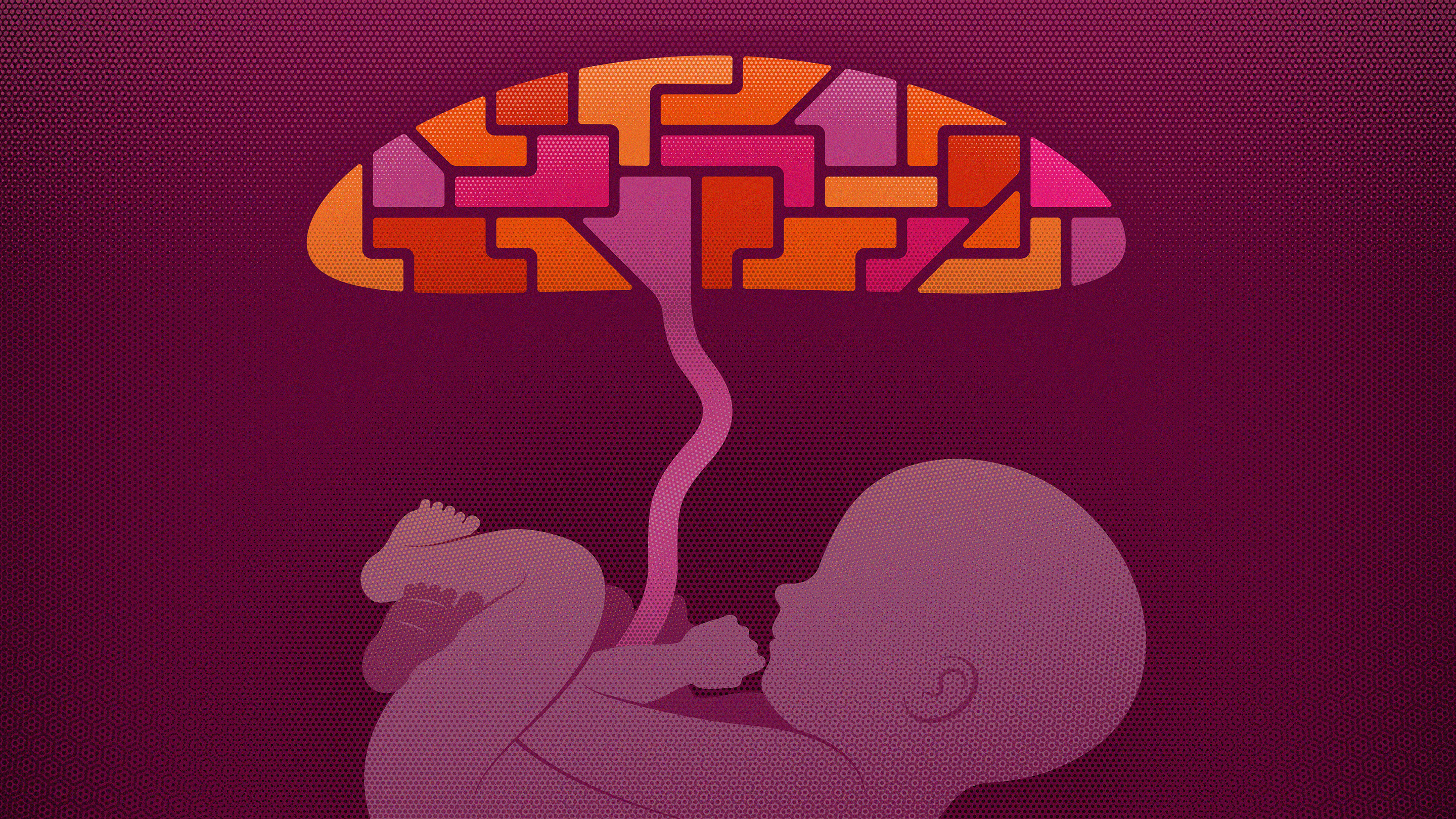
But according to a recent study by Behjati and his colleagues in Nature, human placentas routinely consist of a quilt of different genotypes, and this strange heterogeneity may actually play a role in protecting the fetus from genetic harm. The discovery illuminates not only several mysteries about the placenta itself but also some underlying connections to cancer.
The study painted the clearest picture yet of the genomic landscape of the placenta — and it’s unlike that of any other human tissue ever seen by Behjati, who calls it the “wild west of the human genome.” When they sequenced the DNA of 86 samples from 37 placentas, each set of cells was found to be genetically distinct and chock-full of genetic aberrations typically seen only in aggressive childhood cancers.
“Every placenta is organized as these big chunks of clones that sit next to each other,” he explained. “It’s like a cobblestone pattern of lots of different tumors that together form the placenta, and that is completely astonishing.”
The findings further confirm that the placenta is a biological oddity. Even its origin is peculiar: Placentas are thought to have emerged more than 90 million years ago, when a series of symbiotic retroviruses infiltrated ancient mammals’ genomes and over many generations led to the organ’s formation.
“It’s this strange organ because mothers invest a huge amount of resources into generating the whole placenta, which they then throw away,” said Steve Charnock-Jones, a reproductive biologist at the University of Cambridge and a co-author of the new study. For decades, biologists have puzzled over the apparent wastefulness of this arrangement: Why would natural selection allow a crucial, resource-intensive feature of mammalian life to be so seemingly inefficient?
A Genetic ‘Dumping Ground’
To try to answer this question, Behjati and his colleagues retraced when and where placental cells originate by comparing patterns of mutations in placental samples with samples from corresponding umbilical cords, which develop from fetal cells. The researchers found that cells separate into fetal and placental lineages earlier than anticipated — in some cases, within the first few cell divisions of the zygote. These findings show that the placenta charts its own path separate from that of the fetus early in pregnancy, explained Derek Wildman, an evolutionary biologist at the University of South Florida who was not involved in the study.
But during those crucial first weeks, when a single genetic defect could derail the pregnancy, the placenta may also act as a “dumping ground” for aberrations. During early development, when some of the dividing cells randomly develop genetic abnormalities, they might get earmarked for the placenta instead of the fetus, Behjati reasoned. His team found evidence for this theory: In one of the biopsies, the researchers observed placental cells with three copies of chromosome 10 — two from the mother and one from the father. But cells in the rest of the placenta and fetus had two copies of the chromosome (both from the mother), which suggested that the error started in the fertilized egg but was later corrected.
Patches of the placenta continue to carry on these early mutations — a living archive of genetic defects from the first days of pregnancy — while the fetus remains unharmed. But that’s no problem for the placenta, Wildman hypothesizes, because “it’s not constrained by the necessity to successfully produce an organ that’s going to live for 85 years.” The placenta may not have the same genetic checks and balances that other human cells do because of its inherent transience, he said.
Another possible explanation for these mutations, Behjati said, is that the placenta must outpace the growth of the fetus for the first 16 weeks of human pregnancy, so it may be worth racking up mutations as it balloons inside the uterus. It can “live fast and die young,” as Behjati put it.
Wendy Robinson, a medical geneticist at the University of British Columbia who studies early human development, said that it’s an interesting theory, but she disagreed with the notion that the placenta is merely the genetic garbage pail for the fetus. “There’s very rapid cell divisions that occur early in pregnancy, and that probably imposes a strong selection against cells that just can’t keep up, and so only the good cells will contribute [to the fetus],” she said. “So, it’s not that you’re shunting the bad cells to the placenta — and I know it’s semantics — but it’s that you’re selecting for the good cells in the baby and leaving everything else behind.”
The Normal Abnormal Cells
Regardless of the placenta’s role, the newly uncovered heterogeneity underscores just how miraculous it is that the placenta can evade detection and destruction by the maternal immune system, said Wildman. “You would think that the variant genes, which differ from the maternal genome, would be recognized by the maternal immune system,” he said.
Researchers have long noted similarities between cancers and the placenta — in how they evade the immune system, their invasion tactics and the set of chemical tags on their cells’ DNA that direct the activity of their genes. The two behave alike, too, Robinson said: For a successful pregnancy, the placenta must invade the uterine lining of the mother, tap into the mother’s blood supply and create its own network of blood vessels — all of which cancerous cells do as well.
Given these similarities, “people who study cancer should be very interested in this study,” said Yoel Sadovsky, the executive director of the Magee-Womens Research Institute in Pittsburgh who studies placental genetics. “It may suggest that childhood cancers have the same primitive things as the placenta that allow abnormal cells to propagate, but not in the normal embryonic tissue.”
Although the placenta and cancers are both invasive, there is a crucial difference: The placenta normally knows when to stop growing. (A very rare condition known as placenta accreta occurs if the placenta continues to invade the uterine muscle or nearby organs like the bladder.) While fetal growth accelerates rapidly during the third trimester, the most intense growth for the placenta takes place in the first trimester, said Charnock-Jones, adding that it would be problematic if the placenta continued to act as a tumor and drained valuable resources from the fetus during the third trimester.
“Not only did we find cancer-causing mutations, but we also actually found something that genomically looks like a perfectly normal cancer with very odd genetic signatures and copy number changes,” Behjati said.
“A cell can be normal despite all of that, and I find that quite incredible.”